29.06.2019
Sarcoma of the brain, bones and soft tissues of the head and neck. Tumors of the base of the skull Malignant formation of the bones of the head
Cancer is one of the most terrifying and unpredictable diseases known to medicine. There are many types of cancer pathologies, each of which poses a serious danger to human life. Bone cancer is one of the types of this pathological process that can affect the human body.
According to statistics, cancer of bone structures is the rarest. At the same time, the disease is more often diagnosed in children and adolescents; people over 30 years of age suffer from this form of pathology extremely rarely, in only 2% of cases. Now we will understand what kind of disease this is, what are its causes and symptoms, types, and methods of control.
First of all, it is worth saying that the word cancer itself in medicine means a pathological process in which rapid and uncontrolled division of cells that form a tumor occurs. The neoplasm, wherever it appears, constantly increases in size, affecting nearby tissues. Doctors distinguish only two types of tumors:
- Malignant – the development of a malignant tumor poses the greatest threat to human life, since this type of tumor can spread throughout the body and give metastases. In the final stages of metastasis, malignant cancer cells affect the entire body, the process ends in death.
- Benign – the appearance of benign tumor neoplasms is considered a conditionally safe process. Such tumors grow extremely slowly and do not metastasize; they are removed surgically without further treatment. The neoplasm itself is called benign if it is surrounded by healthy tissue.
Cancer of the joints and skeletal system as a whole “submits” to the same gradation. In addition, there are two separate types of bone cancer:
- Primary – the neoplasm originates directly in the bone tissue. If we are talking about the back, this is the spine, if we are talking about the lower extremities, a certain area of the leg, etc.
- Secondary - cancer begins not in the bones, but in any affected organ in any part of the human body. Over time, at the metastasis stage, metastases appear in the bones, spreading throughout the body from the mentioned organ. The secondary type of bone cancer is more common than the primary one.
It is important to understand that cancer cells can develop in any bone structure. It doesn’t have to be bones; oncology begins in joints, cartilage, and periosteum.
As mentioned earlier, the disease most often affects people under 30 years of age. At this age, as well as in children, oncology is more often localized in the bones of the lower extremities; in older people, the bones of the skull are more likely to be affected.
Causes
Despite the fairly high level of modern medicine and the active study of bone cancer by scientists, the true causes of the development of tumor formations, as well as bone cancer, have not yet been established. Despite this, doctors identify a number of reasons that, in their opinion, predispose or at least precede the development of the disease.
Causes of bone cancer:
- Bone marrow transplantation.
- Exposure of the body to ion radiation, prolonged or repeated exposure to ionizing rays.
- Concomitant genetic diseases, among which the most dangerous are retinoblastoma, Li-Fraumeni or Rothmund-Thompson syndrome.
- Paget's disease, in which the regenerative abilities of bone tissue are impaired, followed by the occurrence of disorders in bone structures.
- The development of primary clinical cancer is facilitated by injuries, mainly bone fractures. In this case, the injury may even be ten years old.
All of the above points relate directly to bone tumors, that is, the primary type of oncology. As for the secondary type of pathology, it is preceded by neoplasms of a different localization. In most cases, we are talking about the most common types of cancer, that is, lung, breast, and prostate cancer metastasizes.
Spine cancer

Despite the fact that spinal cancer has no differences with everything said earlier, it is worth talking about it separately. This is explained by the severe course of tumor formation in the spinal column, because the spinal cord is located here, and the spine itself plays a colossal role in the human body.
In addition, for example, cancer of the thoracic spine will be symptomatically different from the same tumor in another region.
But first of all, it is worth saying that doctors distinguish three separate types of spinal cancer, depending on the location of the tumor:
- Extradural - the tumor is localized outside the dura mater of the spinal cord. Such a tumor often gives metastases, but they do not affect the functions of the central nervous system.
- Intradural – tumor growth occurs directly into the structure of the dura mater. The main danger is compression of the spinal cord, which only aggravates the pathological process.
- Intramedullary - the neoplasm is localized in the spinal cord itself, its enlargement is accompanied by the loss of certain functions. In this case, it all depends on in which part the tumor grows; for example, oncology of the lumbar spine, among other things, threatens paralysis of the lower extremities.
Symptoms of the disease
The development of bone cancer is accompanied by certain symptoms, which become more varied as bone cancer develops and the tumor increases in size.
If we talk about the general clinical picture, the symptoms and manifestations are as follows:
- Pain is the main symptom of cancer. Painful sensations have a clear localization at the site of growth of the malignant tumor. The pain syndrome is constant and does not disappear depending on the position of the body. The pain intensifies with any physical activity, movement, and also at night when the muscles relax.
- Edema - also forms at the site of tumor growth, for example, in one of the lower extremities. The swelling is encircling, it surrounds the tumor, but is clearly visible only when the tumor reaches a significant size. If we are talking about damage to the internal bones in the pelvis or other hard-to-reach area, the swelling may not be visible.
- Deformation of the affected area, which should not be confused with edema, and this is difficult to do. This clinical sign is characterized by protrusion, swelling, swelling of the skin on the affected area of the body. The deformation has the shape of a tubercle, sometimes uneven, its size depends on the size of the growing tumor.
- Impaired motor functions are not always observed, mainly in cases where the tumor is localized near moving joints or structures on which motor functions, innervation of the limbs, etc. depend. A prime example would be cancer of the hip closer to the knee joint. As the tumor grows, it will become more difficult to move your knee, and your leg may become numb or tingly.
- General symptoms of oncology also include signs of causeless weight loss, the appearance of fever (often low-grade), systematic lethargy, loss of appetite, and excessive sweating.
In addition to the general clinical picture, we can identify characteristic symptoms inherent in certain types of bone cancer:

In most cases, the clinical picture of bone cancer is obvious, but only in the later stages. As for the onset of the disease, you should be concerned about any deterioration in your general condition that lasts more than one week.
Types of tumors
As mentioned earlier, doctors distinguish between benign and malignant neoplasms in bone cancer. In addition, the oncological process is characterized depending on the location of the tumor and the characteristics of its course, which affect the principles of treatment. For these reasons, it is worth talking about each type of tumor separately.
Ewing's sarcoma
 This type of neoplasm belongs to malignant ones; it affects mainly tubular bones. It is more common in the lower extremities, spine, pelvis, ribs, collarbone, and shoulder blades.
This type of neoplasm belongs to malignant ones; it affects mainly tubular bones. It is more common in the lower extremities, spine, pelvis, ribs, collarbone, and shoulder blades.
Ewing's sarcoma is diagnosed primarily in people between 10 and 15 years of age. In most cases, the tumor directly affects bone structures, since doctors associate its development with injuries. Extraosseous cases of tissue damage are extremely rare.
Even at the beginning of its development, Ewing's sarcoma can already metastasize, affecting soft tissues, organs, bone marrow, and the central nervous system. For this reason, this type of tumor is considered one of the most aggressive and dangerous.
Osteosarcoma
Osteogenic sarcoma is one of the most common types of bone cancer. The formation of a neoplasm begins with changes in bone structures, develops quickly and gives metastases in the early stages.
In most cases, bone tissue damage occurs in the legs, but there are also known cases of localization in the shoulder girdle and pelvic bones. If we talk about the limbs in general, most often this type of oncology affects the knee or elbow joints in a child’s body.
According to statistics, this type of oncology is more often diagnosed in males. The disease primarily affects people between 10 and 30 years of age, but it is likely to occur at any age. The peak incidence and rate of tumor development occurs during the period of bone growth (adolescence), and is more often diagnosed in tall, tall people.
Chondrosarcoma
 It grows predominantly in cartilaginous tissues or flat bone structures; it has rarely been diagnosed in other bones. The “favorite” location is the area of the larynx and trachea, since small bones are located here.
It grows predominantly in cartilaginous tissues or flat bone structures; it has rarely been diagnosed in other bones. The “favorite” location is the area of the larynx and trachea, since small bones are located here.
There are two scenarios for tumor development:
- Favorable – slow growth with a late stage of metastasis.
- Unfavorable – rapid growth with metastases in the early stages.
It is more often diagnosed in people over 40 years of age, but exceptions are possible.
Fibrosarcoma
It is formed mainly in connective tissues, muscles and tendons, located deep. Only after this the tumor spreads and affects bone tissue. The main place of damage is the legs.
Hondarma
A rare type of cancer, according to some data, developing from embryonic tissues and their residual mass. Localized in the sacrum or bone structures of the base of the skull.
According to its structure, this tumor is considered benign. But due to the specificity of its localization, as well as the high probability of compression of vital nerve branches and organs due to tumor growth, it is regarded as malignant.
Histiocytoma
A malignant neoplasm that affects the upper and lower extremities, trunk, especially the bones in the peritoneal area. Growth occurs in tubular bones of small and large sizes. The neoplasm quickly passes into the stage of metastasis; in most cases, metastases affect the lung tissue.
Parosteal sarcoma
A subtype of osteosarcoma, much rarer and characterized by a less aggressive course. The site of development is the surface of the bone, the growth of the tumor is slow, it is less malignant, so to speak.
In most cases it affects the femur or tibia, in less than 30% of cases it is localized on the bones of the skull, spine, pelvis, hands or feet.
Eosinophilic granuloma
The nature of the development of this type of neoplasm is unknown. According to statistics, this type of tumor most often affects preschool children. The pathology is characterized by numerous foci that “attack” hollow and tubular bones.
The tumors themselves are granulomas, that is, infiltrates, the structure of which contains a high concentration of eosinophilic leukocytes. This type of neoplasm is considered benign.
Chondroblastoma
 Perhaps the most controversial type of neoplasm, as it can be benign or malignant. It is formed from cartilaginous tissue and is formed in different parts of the skeleton in long tubular bones.
Perhaps the most controversial type of neoplasm, as it can be benign or malignant. It is formed from cartilaginous tissue and is formed in different parts of the skeleton in long tubular bones.
Diagnosed in patients over 20 years of age, it is localized in the pelvis, hips, and feet. However, it can develop in the ribs, spine, collarbones, shoulder blades, etc. There is a possibility that after surgery, during which the tumor was not completely removed, it may degenerate into malignant.
Osteoma
It is diagnosed mainly in children and young people under 20 years of age. This type of tumor is benign, it is not prone to rapid growth, does not metastasize, and does not grow into nearby organs and tissues.
Osteomas can form from bone and connective tissue on the humerus, tibia and femur, as well as the thin bones of the skull. Moreover, when osteomas appear, there are no symptoms. The only exceptions are those cases when the tumor reaches a large size and puts pressure on any organ.
Angioma
In most cases, angioma is a vascular formation that is formed from blood or lymphatic vessels. Angioma can also affect bone tissue, but these cases are rare.
Chondromyxoid fibroma
A benign neoplasm that mainly affects long tubular bones, but in rare cases exceptions are possible, with germination in other bone structures. The growth of the tumor is accompanied by painful sensations, and there is a possibility of its degeneration into malignancy.
Chondromyxoid fibroma is a very rare oncological manifestation; in the worst cases, it causes muscle atrophy in the area of localization or limitation of joint mobility, if there is one nearby.
Giant cell tumor
A benign tumor that does not metastasize and is localized in the terminal areas of the bones. In this case, the tumor often grows into nearby tissues, and its main disadvantage is that even after surgical removal of the tumor, it can grow again.
Osteoid osteoma
A single benign formation that does not grow more than 1 centimeter in diameter. The tumor can develop in any bone structure of the human skeleton. Moreover, osteoid osteoma is rarely diagnosed, since it is small, and when it appears there are no symptoms.
Stages of bone cancer
Recognizing the stage of development of the pathological process plays a decisive role in setting up treatment, and sometimes predicting life. In total, there are 4 stages of bone cancer development:
- Education does not leave the bone. Tumors at the first stage are divided by size, above and below 8 centimeters.
- The tumor is still localized only within the bone, but tests confirm signs of cellular malignancy.
- The tumor spreads to several bone structures, and cancer cells penetrate into the area of regional lymph nodes.
- The fourth stage is characterized by the growth of the tumor beyond the bone, onto nearby tissues. With stage 4 bone cancer, the process of metastasis begins.
Diagnostics
 Bone cancer always requires diagnosis. To do this, you need to consult a doctor, who will prescribe the necessary diagnostic measures. Diagnosis is necessary to identify cancer cells in principle, determine the stage of development of oncology, and prescribe treatment.
Bone cancer always requires diagnosis. To do this, you need to consult a doctor, who will prescribe the necessary diagnostic measures. Diagnosis is necessary to identify cancer cells in principle, determine the stage of development of oncology, and prescribe treatment.
Diagnostic methods are as follows:
- The first thing to do is to take an x-ray of the bones at the suspected location of the tumor.
- The patient must undergo a blood test to detect tumor markers for cancer.
- Isotope scanning - a special substance is injected into the bloodstream, which is absorbed by bone tissue. Then a special scanner is used to “highlight” the substance in the bones and detect even the smallest formations.
- Computed and magnetic resonance tomography.
- A biopsy of tumor tissue to determine the type of tumor (malignant or benign).
How to treat bone cancer
Treatment of any cancer is a complex and painstaking process, especially for bone cancer. Cancer should be treated only by contacting an oncologist, who will make a diagnosis and prescribe a treatment regimen based on the diagnostic data obtained.
It is important to understand that for each patient and specific case of the disease, treatment is prescribed individually. For some, this means radiation and chemotherapy, but in most cases they still resort to surgical removal of the tumor or part of the bone. In the second case, the bone is subsequently replaced by a special prosthesis. In especially difficult situations, a decision is made together with the patient to amputate the affected limb.
How long do you live with bone cancer?
The life expectancy of people with bone cancer is, again, controversial and has a huge number of variables. It is necessary to take into account the location of the tumor, the stage of its development, the type of tumor, the presence or absence of metastases, the age of the patient, etc.
Of course, the most favorable prognosis will be if the cancer was detected at the first stage and the tumor was completely removed. After this, irradiation is carried out and the survival rate exceeds 80%. The higher the stage of cancer, the more unfavorable factors, the lower this figure.
(1
ratings, average: 5,00
out of 5)
Tumors of the skull base are neoplasms that have a different histological structure and can be localized in the cranial cavity or in the area of the facial skeleton. Most often, tumors of the skull base are metastases of other malignant neoplasms.
The base of the skull is the bottom of the cranium, formed by several bones (basal, occipital, frontal and temporal). The base of the skull appears in the human embryo already in the second month of its embryonic life. The definition of “tumor of the skull base” is collective and combines various pathological processes that affect this anatomical formation.
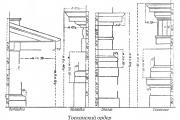
Anatomy
Inner base of the skull- This is the surface of the skull that faces the medulla. The inner base of the skull follows the contours of the adjacent brain. It is permeated with holes and channels - blood vessels and cranial nerves pass through them.
The surface has three depressions - the anterior, middle and posterior cranial fossae. The cerebrum is located in the anterior and middle fossa, and the cerebellum is located in the posterior fossa. The anterior and middle fossae are separated by the posterior edges of the small wings of the sphenoid bone, the middle fossa is separated from the posterior dorsum of the sella turcica and the upper edge of the pyramids of the temporal bones.
- The anterior cranial fossa contains the frontal lobes of the brain. It communicates with the nasal cavity and is located in the area of the frontal and ethmoid bones.
- The middle one is located in the area of the sella turcica and communicates with the orbits through the optic canals. The pituitary gland is located in the central part of the middle cranial fossa, and the temporal lobes of the hemispheres are located in the lateral parts. In front of the sella turcica lies the optic chiasm.
- The posterior cranial fossa is located in the region of the temporal and occipital bones and communicates with the spinal canal through the large foramen.
External base of the skull has a large number of openings - nerves and vessels (arteries, veins) pass through them. In front it is covered by the bones of the facial part of the skull. The posterior section of the outer base of the skull is formed from the outer surfaces of the temporal, sphenoid and occipital bones.
Since there is both an external and internal base of the skull, we include not only pathological processes in the internal base, but also formations located in the structures that make up the external base of the skull as tumors of the skull base. Major advances in the treatment of tumors of the skull base have occurred due to the discovery of new diagnostic methods - computed tomography and MRI (magnetic resonance imaging). Without the use of these examination methods, the likelihood of a clinical error is very high: small tumors that occur without symptoms can immediately affect the base of the skull and, accordingly, pose a significant threat to the patient’s life. Tumors that produce much more severe symptoms may not spread directly to the base of the skull and have a much better prognosis.
Etiology and pathogenesis
Tumors of the skull base are most often of a metastatic nature. Most often, the primary sources of metastases are malignant breast tumors, lung cancer, multiple myeloma and prostate cancer. Damage to the base of the skull can result from contact spread of nasopharyngeal cancer, osteosarcoma, squamous cell carcinoma, glomus tumors, and chordoma. All of these tumors can spread to the base of the skull. Separately, we can highlight formations that are within the competence of otoneurologists, otolaryngologists and rhinologists: tumors localized in the nasal cavity, nasopharynx and sinuses.
Tumors affecting the base of the skull can be either malignant or benign. An example of a benign tumor with such a localization is meningioma.
Symptoms and course
A tumor of the base of the skull is a rare and complex pathology. For the most part, tumors of the skull base are represented by metastases of malignant tumors in other parts of the body - mammary glands, lungs, prostate gland. Another reason for the development of this condition is a tumor process in the paranasal sinuses.
Tumors of the base of the skull are accompanied by manifestations of organic brain damage - headache, fainting, epileptic seizures and other neurological symptoms. When the tumor spreads into the cranial cavity and orbit, in addition to neurological disorders, ophthalmological disorders also appear - vision problems.

An even less common occurrence is the development of a primary tumor directly from the bones that make up the base of the skull. Due to the rarity of the pathology and the blurred clinical picture, the disease is extremely rarely detected in a timely manner. The possibility of radical surgical intervention with such data is very difficult, since:
- The tumor often spreads into the cranial cavity
- The pathological process involves the brain and cranial nerves
- Several anatomical zones are affected at once
If the formation is located in the area of the nose or nasopharynx, then it causes the following clinical picture:
- Headache
- Facial pain
- Nasal breathing problems
- The appearance of mucous or bloody discharge from the nose
- Symptoms of sinusitis
From the appearance of the first signs of the disease to the full clinical picture, it can take from six months to a year - in each case the disease develops individually. If the complaints listed above occur, the patient should immediately consult a doctor, because if there is a delay, his health may be seriously affected (tumors of the base of the skull can be fatal).
Diagnostics
Initial examination by a doctor
The doctor listens to the patient’s complaints, finds out how the disease manifests itself clinically, and collects anamnesis.
Instrumental diagnostic methods
- Endoscopic examination of the nasal cavity
- X-ray computed tomography (CT)
- Magnetic resonance imaging (MRI)
However, despite the high level of modern devices, the likelihood of a diagnostic error still remains quite high.
Listed below are specific diagnostic methods that allow you to eliminate doubts and make the correct diagnosis.
- Neurosurgical biopsy
- Tumor resection followed by histological examination
Treatment
Extended combined operations, which are indicated for such complex pathologies, can lead to serious complications and sometimes fatal outcomes. Therefore, an important task of modern medicine is to find effective, and at the same time, organ-preserving methods of treating tumors of the base of the skull.
Radiation therapy is recommended for patients with a tumor at the base of the skull. An innovative method of treating such formations is stereotoxic radiosurgery and the CyberKnife installation. "Cyber Knife" is a high-precision treatment method equipped with a moving arm, a manipulator and robotics. Treatment with the installation does not require hospitalization; procedures can be performed on an outpatient basis.
Tumors of the skull bones. divided into primary and secondary (germinating or metastatic), characterized by benign or malignant growth. Among primary benign tumors of the calvarial bones, the most common are osteomas and hemangiomas. Osteoma develops from the deep layers of the periosteum. Its occurrence is associated with a violation of embryonic development and hand formation. With growth, a compact osteoma is formed from the outer and inner plates of the kernel substance, and a spongy (spongy) or mixed form of osteoma is formed from the spongy substance. The development of osteoid osteoma is also possible. Osteomas, as a rule, are single, less often - multiple. In the bones of the skull. Compact osteomas predominate. They are characterized by slow growth, may not appear clinically for a long time, and are sometimes accidentally discovered during X-ray examination. If clinical symptoms are present, surgical treatment is removal of the osteoma. The prognosis is favorable. Hemangioma of the skull bones is rare.
Localized in the spongy substance of the frontal and parietal (less often occipital) bones. In the bones of the cranial vault. Usually a capillary (spotted) hemangioma develops, less often a cavernous or racemotic form. Clinically, hemangioma is often asymptomatic and detected incidentally on an x-ray. In this case, the integrity of the bone plate, which is important for radiation or surgical treatment, is clarified using axial computed tomography data. Benign neoplasms in the soft tissues of the head can secondary locally destroy the bones of the cranial vault. Dermoid cysts are usually located at the outer and inner corner of the eye, in the area of the mastoid process, along the sagittal and coronal sutures, etc. They are located under the aponeurosis, which causes the development of skull bone defects, saucer-shaped marginal defects, followed by complete destruction of all layers of the bone. In rare cases, a dermoid cyst develops as a diploe on cranial radiographs. a cavity with smooth walls is visible. Eosinophilic granuloma or Taratynov's disease is characterized by local bone destruction caused by the intraosseous development of granulomas consisting of histiocytic cells and eosinophils. Usually a solitary bone granuloma is detected, less often - several foci, and very rarely - multiple skeletal lesions. Most often these changes are localized in the flat bones of the skull and the femur.
The flat bones of the pelvis, ribs, vertebrae, and jaws may be affected. Treatment of benign tumors is surgical. The prognosis is favorable. Cholesteatoma can be located in the soft tissues of the head, most often under the aponeurosis. In this case, extensive defects of the outer bone plate and diploe are formed with clear scalloped edges and a marginal band of osteosclerosis. Cholesteatoma located in the diploea is radiologically identical to a dermoid or teratoma. Treatment is surgical. The prognosis is favorable. To primary malignant tumors of the calvarial bones. include osteogenic sarcoma. However, secondary sarcoma is more common, developing from the periosteum, dura mater of the brain, aponeurosis and paranasal sinuses.
Sarcomas develop at a young age, are large in size and have a slight tendency to decay, quickly invade the dura mater and give metastases. On the radiograph, the lesion has an uneven outline, with borderline osteosclerosis; When the tumor grows beyond the cortex, radiant periostitis appears in the form of fan-shaped diverging bone spicules. Since osteogenic sarcoma develops from primitive connective tissue capable of forming bone and tumor osteoid, the X-ray picture combines osteolytic and osteoblastic processes, which is clearly visible on computed tomograms. Antitumor drugs and radiation therapy are prescribed, and in some cases surgical treatment is indicated. The bones of the calvarium are affected in myeloma in the form of a solitary lesion (plasmocytoma); diffuse damage is less common.
At the same time, pathological foci can be detected in the ribs, pelvic bones, spine, tubular bones, and sternum. A disorder of protein metabolism in the form of paraproteinemia is characteristic: a-, b- and g-plasmocytomas are differentiated by an increase in the amount of globulins. Sometimes the tumor grows into adjacent tissue (for example, into the dura mater of the brain). The main clinical symptom is pain in the affected bones. The diagnosis is established on the basis of clinical and laboratory data, the results of a bone marrow punctate examination and an x-ray picture. Treatment consists of prescribing antitumor drugs and radiation therapy. Sometimes surgery is indicated.
The prognosis is unfavorable. Metastasis to the bones of the calvarium is observed in primary cancer of the lung, breast, thyroid and parathyroid glands, kidney, and prostate. Foci of bone destruction are localized in the cancellous bone and have a wide zone of sclerosis, which moves outward as the metastasis increases. Metastases of kidney adenocarcinoma are characterized by local bone destruction with the formation of intra- and extracranial nodes. Multiple lytic small-focal metastases of different configurations in the bones of the calvarium, reminiscent of multiple foci in multiple myeloma, are observed in malignant chromaffinoma of the adrenal glands, mediastinum, and liver.
Inna Bereznikova
Reading time: 7 minutes
A A
Everyone knows what a skull is, but only a few understand where its base is. Let's try a quick anatomy course to clear things up. This is a very complex system, consisting of posterior and anterior sections. The anterior one, in turn, is characterized by a boundary location between the organs of the face and the brain, and the posterior one - between the cervical region and the brain. In more understandable language: the anterior section of the base of the skull is located in the area of the paranasal sinus, and the posterior section is located in the occipital part.
Tumors of the base of the skull are a fairly rare occurrence. Treating such a disease is very difficult and dangerous, but the neglected process brings even more trouble. It is better to get rid of the formation as soon as you notice the first symptoms.
Inner base of the skull
Types of benign tumors of the skull base:
- inverted papilloma;
- polyps;
- meningioma;
- fibroma;
- osteoma;
- schwannoma;
- neurofibroma;
- cementoma;
- Thornwald's bag.
Most often, benign occurs, since it is in this part that the maximum amount of fatty tissue is concentrated, which is constantly exposed to mechanical stress. Let's look at the most popular formations.
Inverted papilloma
This is a benign tumor of the base of the skull, which is located in the paranasal sinuses. It begins to develop at the age of 50, affecting mostly men. Education has local aggressiveness. Under the influence of inverted papilloma, soft tissues suffer and the dense bone walls of the nose are partially destroyed. The main danger of inverted papillomas is the tendency to frequent relapses. Also, about 5% of formations degenerate into cancer.
Diagnostics
Papillomas are diagnosed by assessing the symptoms of their manifestation. Let's consider the main ones:
- difficulty breathing in one of the nasal sinuses or its complete absence;
- if the tumor is enlarged, it may be opened, resulting in nosebleeds;
- the functions of smell are impaired;
- which gradually spread to the entire face;
- constant heaviness in the nasal passage;
- excessive tearing;
- deformation of the external nasal cartilages.
After assessing the symptoms, they proceed to a hardware examination. Rhinoscopy or computed tomography is prescribed, which show the internal structure of the formation. It has a granular structure and is located in the area of the base of the skulls in peculiar lobules. Upon closer examination, papillary growths are revealed. The color of the inverted papilloma tissue is pink or purplish red.

Treatment
Inverted papilloma can only be cured through surgery. The endoscopic method is often used. This is contact removal in a single block for less invasiveness. The main thing is not to destroy the surrounding mucous membranes. After surgery, it is very important to undergo examination every six months in order to exclude the possibility of relapse.
Meningioma
This is a benign tumor of the base of the skull that can transform into a malignant tumor over time. Grows from the hard tissues of the meninges. Characterized by slow growth and gradual expansion. As a rule, it is very difficult to completely remove such a formation, so all patients who have undergone surgery are recommended to carry out regular diagnostics to exclude malignancy of the formation. Also like this. Meningiomas occur most often at the age of 35 years.
Degrees of development of meningiomas:
- benign first degree;
- atypical second degree;
- malignant third degree.
The main cause of the development of meningiomas is radiation exposure. A similar tumor can also develop after radiation therapy, which is used to treat many types of cancer.
Symptoms
The disease manifests itself depending on its location and size. At first, meningioma can grow asymptomatically, but as it grows it causes considerable discomfort.
Diagnostics
Diagnosis of the disease cannot be made without a visual examination. The general condition, symptoms of meningioma, as well as reflex reactions and sensitivity of the skin are assessed. The patient also undergoes consultation with an ENT specialist and an ophthalmologist. MRI and computed tomography are performed. A biopsy helps determine the benign origin of the tumor, but it can only be done during surgery.
Treatment
After a diagnostic examination, treatment tactics are determined. As a rule, surgical intervention is prescribed. As preparation, the patient is given conservative treatment to reduce the tumor and slow down its development. Inflammatory processes are also relieved with the help of corticosteroid drugs.
Schwannoma (neurinoma)
A benign formation that forms from peripheral and spinal nerves. It is the result of the proliferation of the myelin sheath in the cavity of the base of the skull. Occurs at the age of 50 years. Outwardly it resembles a dense round formation with an outer framing shell. The growth rate is quite slow: 1-2 mm annually. With more intensive growth, a suspicion arises about the malignancy of the formation.
Causes
Reasons for development:
- radiation exposure to which the body is exposed at an early age;
- long-term influence of chemical fumes;
- harmful working conditions;
- genetic neurofibromatosis heredity;
Symptoms
Symptoms of the disease appear depending on the location and size of the formation. The tumor can affect the optic nerves, the hearing aid, and cause cerebellar disorders.

First symptoms:
- if the auditory nerve is involved in the tumor process, a constant ringing occurs in the ears;
- hearing is impaired;
- Coordination is impaired and severe dizziness occurs.
Later manifestations:
- when the formation grows to 2 cm, the trigeminal nerve is compressed;
- the sensitivity of the facial skin is impaired;
- dull pain in the affected area. Often the patient confuses it with a tooth;
- When the tumor grows to 4 cm, the facial nerves begin to be compressed, causing loss of taste, excessive salivation, and strabismus.
Posterior fossa tumors
Such formations include pathological changes in brain tissue, the fourth ventricle and medulla oblongata. There are meningiomas, astrocytomas, neuromas, and gliomas. Such formations appear at an early age, develop slowly and can transform into cancer. If posterior fossa tumors occur in old age, this is usually the result of metastases.
Symptoms
Symptoms of tumors of the posterior cranial fossa:
- frequent nausea and causeless vomiting;
- headache that does not go away after taking painkillers;
- deterioration of hearing and vision;
- numbness of the face and neck, pain in the same area;
- damage to the central nervous system;
- the appearance of unusual tics;
- dizziness;
- changes in facial appearance;
- violation of the swallowing reflex.
Diagnostics
Diagnosis of a tumor of the posterior cranial fossa is carried out according to the assessment of the symptoms described by the patient, as well as using hardware examination. Since the formation begins to manifest itself only at later stages with an increase in volume, it is impossible to do without X-rays, MRI and computed tomography.
- X-ray is the simplest diagnostic method and shows the level of damage to the bone part of the skull;
- computed tomography using x-ray radiation allows you to accurately determine the contours of the tumor and the level of penetration deep into the nervous system;
- MRI is an important diagnostic procedure that provides high-quality information about pathological transformations of soft tissues;
- cerebrospinal fluid puncture assesses damage to the nervous system, as well as the extent of its prevalence;
- electroencephalography demonstrates the basic functionality of the nervous system;
- genetic testing indicates that the patient has hereditary neurofibromatosis;
- histology helps to establish an accurate diagnosis and prescribe effective treatment.

Surgery for skull base tumors
Treatment
The success of treatment depends on the experience and dexterity of the neurosurgeon, since in most cases it is not possible to avoid surgical intervention. This is a radical method of getting rid of education. The main goal is not to affect the central nervous system. In modern medicine, microsurgical instruments with a special optical system are used. This is the only way to carry out the operation with extreme precision. Doctors try to avoid damage to healthy tissue and the development of serious complications.
Skull bone tumors divided into primary and secondary (germinating or metastatic), characterized by benign or malignant growth. Among primary benign tumors of the calvarial bones, the most common are osteomas and hemangiomas. Osteoma develops from the deep layers of the periosteum. Its occurrence is associated with a violation of embryonic development and hand formation. With growth, a compact osteoma is formed from the outer and inner plates of the kernel substance, and a spongy (spongy) or mixed form of osteoma is formed from the spongy substance. The development of osteoid osteoma is also possible. Osteomas, as a rule, are single, less often - multiple. In the bones of the skull... compact osteomas predominate. They are characterized by slow growth, may not appear clinically for a long time, and are sometimes accidentally discovered during X-ray examination. If clinical symptoms are present, surgical treatment is removal of the osteoma. The prognosis is favorable.
Hemangioma of the skull bones is rare. Localized in the spongy substance of the frontal and parietal (less often occipital) bones. In the bones of the cranial vault. Usually a capillary (spotted) hemangioma develops, less often a cavernous or racemotic form. Clinically, hemangioma is often asymptomatic and detected incidentally on an x-ray. In this case, the integrity of the bone plate, which is important for radiation or surgical treatment, is clarified using axial computed tomography data.
Benign neoplasms in the soft tissues of the head can secondary locally destroy the bones of the cranial vault.
Dermoid cysts They are usually located at the outer and inner corners of the eye, in the area of the mastoid process, along the sagittal and coronal sutures, etc. They are located under the aponeurosis, which causes the development of skull bone defects, saucer-shaped marginal defects, followed by complete destruction of all layers of the bone. In rare cases, a dermoid cyst develops into a diploe on radiographs of the skull... a cavity with smooth walls is visible.
Eosinophilic granuloma or Taratynov's disease characterized by local bone destruction caused by the intraosseous development of granulomas consisting of histiocytic cells and eosinophils. Usually a solitary bone granuloma is detected, less often - several foci, and very rarely - multiple skeletal lesions. Most often these changes are localized in the flat bones of the skull and the femur. The flat bones of the pelvis, ribs, vertebrae, and jaws may be affected. Treatment of benign tumors is surgical. The prognosis is favorable.
Cholesteatoma can be located in the soft tissues of the head, most often under the aponeurosis. In this case, extensive defects of the outer bone plate and diploe are formed with clear scalloped edges and a marginal band of osteosclerosis. Cholesteatoma located in the diploea is radiologically identical to a dermoid or teratoma. Treatment is surgical. The prognosis is favorable.
Primary malignant tumors of the bones of the cranial vault include... osteogenic sarcoma. However, secondary sarcoma is more common, developing from the periosteum, dura mater of the brain, aponeurosis and paranasal sinuses. Sarcomas develop at a young age, are large in size and have a slight tendency to decay, quickly invade the dura mater and give metastases. On the radiograph, the lesion has an uneven outline, with borderline osteosclerosis; When the tumor grows beyond the cortex, radiant periostitis appears in the form of fan-shaped diverging bone spicules. Since osteogenic sarcoma develops from primitive connective tissue capable of forming bone and tumor osteoid, the X-ray picture combines osteolytic and osteoblastic processes, which is clearly visible on computed tomograms. Antitumor drugs and radiation therapy are prescribed, and in some cases surgical treatment is indicated.
The bones of the cranial vault are affected by multiple myeloma in the form of a solitary focus (plasmocytoma); diffuse damage is less common. At the same time, pathological foci can be detected in the ribs, pelvic bones, spine, tubular bones, and sternum. A disorder of protein metabolism in the form of paraproteinemia is characteristic: a-, b- and g-plasmocytomas are differentiated by an increase in the amount of globulins. Sometimes the tumor grows into adjacent tissue (for example, into the dura mater of the brain). The main clinical symptom is pain in the affected bones. The diagnosis is established on the basis of clinical and laboratory data, the results of a bone marrow punctate examination and an x-ray picture. Treatment consists of prescribing antitumor drugs and radiation therapy. Sometimes surgery is indicated. The prognosis is unfavorable.
Metastasis to bone of the cranial vault is observed in primary cancer of the lung, breast, thyroid and parathyroid glands, kidney, and prostate. Foci of bone destruction are localized in the cancellous bone and have a wide zone of sclerosis, which moves outward as the metastasis increases. Metastases of kidney adenocarcinoma are characterized by local bone destruction with the formation of intra- and extracranial nodes. Multiple lytic small-focal metastases of different configurations in the bones of the calvarium, reminiscent of multiple foci in multiple myeloma, are observed in malignant chromaffinoma of the adrenal glands, mediastinum, and liver.



 This type of neoplasm belongs to malignant ones; it affects mainly tubular bones. It is more common in the lower extremities, spine, pelvis, ribs, collarbone, and shoulder blades.
This type of neoplasm belongs to malignant ones; it affects mainly tubular bones. It is more common in the lower extremities, spine, pelvis, ribs, collarbone, and shoulder blades. It grows predominantly in cartilaginous tissues or flat bone structures; it has rarely been diagnosed in other bones. The “favorite” location is the area of the larynx and trachea, since small bones are located here.
It grows predominantly in cartilaginous tissues or flat bone structures; it has rarely been diagnosed in other bones. The “favorite” location is the area of the larynx and trachea, since small bones are located here. Perhaps the most controversial type of neoplasm, as it can be benign or malignant. It is formed from cartilaginous tissue and is formed in different parts of the skeleton in long tubular bones.
Perhaps the most controversial type of neoplasm, as it can be benign or malignant. It is formed from cartilaginous tissue and is formed in different parts of the skeleton in long tubular bones. Bone cancer always requires diagnosis. To do this, you need to consult a doctor, who will prescribe the necessary diagnostic measures. Diagnosis is necessary to identify cancer cells in principle, determine the stage of development of oncology, and prescribe treatment.
Bone cancer always requires diagnosis. To do this, you need to consult a doctor, who will prescribe the necessary diagnostic measures. Diagnosis is necessary to identify cancer cells in principle, determine the stage of development of oncology, and prescribe treatment.