12.04.2019
Complicated obstetric history. History during gynecological examination
Currently, clinical, laboratory, instrumental, and endoscopic methods studies that allow the doctor to determine the state of the female body and identify disorders leading to disorder of the woman’s health.
Taking a history of a gynecological patient
The examination of a gynecological patient begins with anamnesis. Its purpose is to identify the main complaints, obtain information about previous life and previous diseases, and the development of this disease.
Survey carried out in a certain sequence. First, they find out general information: last name, first name, patronymic, marital status, profession, age, living conditions and food, bad habits sick.
Age is important, since the same symptom at different periods of a woman’s life can be a manifestation of different diseases.
Finding out the patient’s profession and working conditions helps clarify the causes of many pathological processes. For example, work associated with prolonged cooling or overheating can lead to an exacerbation of the inflammatory process.
After receiving general information the patient should be asked about the complaints that forced her to see a doctor. Complaints upon admission are clarified without excessive detail, since in the future they are clarified by identifying the characteristics of the specific functions of the female body (menstrual, sexual, reproductive and secretory) and the history of the present disease.
Typically, gynecological patients complain of pain, leucorrhoea, menstrual cycle disorders (usually uterine bleeding), and infertility. Pain is a symptom accompanying many gynecological diseases. They vary in intensity, localization, character (constant, aching, cramping, gnawing), and irradiation.
When collecting anamnesis, attention should be paid to heredity. The presence of chronic infections (tuberculosis, etc.), mental, venereal, tumor diseases, and blood diseases in parents or close relatives helps to determine the patient’s predisposition to these diseases.
The patient's interview includes finding out her life history, starting from an early age. Of particular importance in identifying the causes of gynecological diseases are common diseases in past. Frequent sore throats, rheumatism, liver diseases, neuroinfections and other diseases often lead to disorders menstrual function, retardation in physical and sexual development.
Obstetrics gynecological history
includes information about the features of specific functions of the female body: menstrual, sexual, reproductive and secretory.
The survey should begin with finding out the time of the first menstruation (menarche), the type of menstrual function (duration menstrual cycle and menstruation, the amount of blood lost, pain), dates of the last menstruation.
Peculiarities of sexual function are closely related to gynecological diseases: the onset of sexual activity, sexual sensation, sexual intercourse disorders (pain, the appearance of bloody discharge after sexual intercourse), methods of preventing pregnancy (contraception). The age and health status of the husband may play a role in establishing the diagnosis. When clarifying the nature of childbearing function, information is carefully collected on the number of pregnancies, their course and outcome. If the patient complains of infertility, you should find out what studies and treatment were previously carried out.
Character secretory function determined by obtaining data on the presence of pathological discharge (leucorrhoea) from the genital tract and its quantity. The causes of leucorrhoea are most often inflammatory diseases of the vulva, vagina, cervix and overlying organs of the reproductive system of various etiologies. Besides inflammatory diseases leucorrhoea can be a sign of polyp and uterine cancer. They can be thick, liquid, watery, purulent, ichorous, and sometimes cause itching in the area of the external genitalia and vagina.
Often a symptom of a gynecological disease is dysfunction of the urinary tract and intestines. Therefore, when interviewing the patient, it is necessary to inquire about the condition of these adjacent organs. Information about previous gynecological diseases, their course, outcome, treatment, including surgical interventions, should be clarified in detail.
After establishing the characteristics of the obstetric and gynecological history, they proceed to history of the present illness. Particular attention is paid to information about the development of the present disease: the time of occurrence, connections with abortion, childbirth, menstruation and other factors, the nature of the treatment and its results. After the interview, the doctor has sufficient information to make a preliminary conclusion about the nature of the disease. To further clarify the diagnosis, an objective examination of the patient is necessary.
Objective research methods in gynecology
General research allows you to get an idea of the state of the body as a whole. It includes a general examination (body type, condition of the skin and mucous membranes, nature of hair growth, condition and degree of development of the mammary glands), examination of organs and systems using generally accepted medical methods.
Particular attention is paid to examining the patient's abdomen. In addition to examination, methods of palpation, percussion and ascultation of the abdomen are used, which often give rise to the assumption of a gynecological disease. Further general examination of the patient consists of measuring body temperature, blood pressure, as well as laboratory testing of blood, urine, feces, etc.
Special research methods Gynecological patients are numerous and vary in purpose and degree of complexity.
A gynecological examination of the patient is carried out in horizontal position on a gynecological chair or hard couch. The head end of the chair must be raised, the legs bent at the knees and widely spread to the sides are held in place by leg holders. A woman must be previously prepared for a gynecological examination. If she does not have stool, a cleansing enema is given in advance.
Immediately before the test, she should have a bowel movement. bladder, and if spontaneous urination is delayed, the nurse, as prescribed by the doctor, removes urine using a catheter. For examination, the nurse must prepare sterile instruments: vaginal speculum, tweezers, forceps, probes, as well as glass slides for taking smears, sterile cotton balls and gauze napkins. Examination of gynecological patients is carried out wearing sterile rubber gloves.
Gynecological examination begins with examination of the external genitalia, in which attention is paid to the type of hair growth, the structure of the labia majora and minora, the condition of the external opening of the urethra, the excretory ducts of the paraurethral and large glands of the vestibule, perineum and anus. To examine the vestibule of the vagina, spread the labia with the thumb and index fingers of the left hand. Pay attention to the gaping of the genital slit. The presence of prolapse or prolapse of the walls of the vagina and uterus is determined when the patient strains.
Research using mirrors performed after examination of the external genitalia. There are various models of vaginal speculum, among which the most commonly used are bicuspid self-supporting and spoon-shaped speculums. The use of a double-leaf mirror does not require an assistant, so it is used more often in outpatient practice.
The nurse should know the rules for inserting a speculum. Before inserting the speculum, the labia are spread apart with the index finger and thumb of the left hand. The double-leaf speculum is inserted closed in straight size to the middle of the vagina. Next, the mirror is turned to a transverse size and advanced to the fornix, opening the valves, as a result of which the cervix becomes accessible for inspection. The spoon-shaped speculum is first inserted with its edge along the posterior wall of the vagina, and then, having been inserted into the depths, it is turned across, pushing the perineum backwards.
In parallel, an anterior speculum-lift is inserted, which is used to lift the anterior wall of the vagina. When examining with mirrors, the shape of the cervix is determined (conical in a nulliparous woman, cylindrical in a woman who has given birth, deformed), its position, size, color of the mucous membrane, and the presence of pathological processes. The walls of the vagina are examined by gradually removing the speculum.
Vaginal (internal examination) performed after examination using mirrors with the index and middle fingers or only the index finger of one hand (usually the right). A vaginal examination allows you to determine the condition of the perineum, pelvic floor muscles, urethra, large glands of the vestibule, vaginal walls and the vaginal part of the cervix.
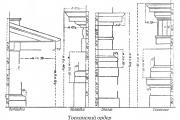
Rice. 69. Two-handed (vaginal-abdominal) examination
Two-manual vaginal (bimanual, vaginal-abdominal) examination is the main method for diagnosing diseases of the uterus, appendages, pelvic peritoneum and fiber (Fig. 69). It is carried out in a certain sequence. First of all, the uterus is examined, determining its position, size, shape, consistency, mobility, and pain.
During a two-handed examination, the uterus moves within certain limits up, down, anteriorly and to the sides, but then returns to its original position, which determines the physiological nature of this mobility. Then they begin to examine the uterine appendages. To do this, the fingers of both hands (outside and inside) are gradually moved from the corners of the uterus to the side walls of the pelvis. Unchanged fallopian tubes are usually not palpable, and the ovaries can be palpated in the form of small ovoid formations. A two-handed examination also makes it possible to identify pathological processes in the area of the pelvic peritoneum and the tissue of the pelvic ligaments.
Rectal and rectal-abdominal examination used in virgins, for atresia or stenosis of the vagina, as well as for inflammatory or tumor processes in the reproductive system. The examination is carried out wearing a rubber glove with a fingertip, which is lubricated with Vaseline.
Rectal-vaginal examination is used for diseases of the posterior wall of the vagina or the anterior wall of the rectum. In this case, the index finger is inserted into the vagina, and the middle finger of the right hand is inserted into the rectum.
Additional research methods in gynecology
All women admitted to the gynecological hospital are subjected to bacterioscopic examination. Discharges from the lower parts of the genitourinary system - vagina, cervical canal and urethra - are subject to examination. A nurse working in a hospital or antenatal clinic must master the technique of correctly taking smears. First of all, the nurse should warn the patient that on the eve and on the day of taking smears she should not have sexual intercourse or douche.
She should also not urinate for 2 hours before taking swabs. The nurse needs to prepare two glass slides, well washed, wiped with alcohol or ether and dried. Using a special pencil, each glass is divided into three parts, on one of which the letter U is written, which means urethra, on the second C - cervix, on the third V - vagina.
When taking material from various parts of a woman’s genital organs, the nurse should: remember the need to carefully observe the rules of asepsis and antisepsis. Only sterile instruments are used, and the same instrument cannot be used to take smears from different places. Smears are taken before a gynecological examination of the patient, as well as before vaginal medical procedures.
To obtain smears, the woman is placed on a gynecological chair. First, swabs are taken from the urethra; To do this, gently massage it with a finger inserted into the vagina. The first portion of discharge from the urethra should be removed with a cotton ball, and then a grooved probe, the tip of tweezers or a special spoon (Volkmann) should be inserted into the urethra (to a depth of no more than 1.5-2 cm). The material from the urethra is obtained by lightly scraping and applied in the form of a circle on two glass slides with a U mark.
After taking smears, a sterile speculum is inserted from the urethra into the vagina, the cervix is exposed, and after wiping it with a cotton ball with a sterile instrument, a smear is taken from the cervical canal in the same way as from the urethra. Light scraping is necessary so that the test material gets gonococci, which are usually located not on the surface of the mucous membrane, but under the epithelial cover. Next, the discharge is taken from the posterior vaginal fornix with tweezers or a forceps.
Discharge from the cervix and vagina is applied separately as a streak onto glass slides with the appropriate mark. The smears are dried and then sent with an accompanying note to the laboratory. In the laboratory, smears are stained with methylene blue on one slide, and Gram stained on the second, after which they are subjected to microscopic examination. During bacterioscopic examination of smears from the posterior vaginal fornix, the degree of purity of the vaginal contents is determined. Smears from the urethra and cervical canal are used for bacterioscopic examination for gonococci and flora.
If necessary, the secretion of the vestibular glands and rectum can be subjected to bacterioscopic examination. Patients who are suspected of having gonorrhea undergo a so-called provocation. Under provocation understand special measures of influence on a woman’s body, aimed at exacerbating the inflammatory process of gonorrheal origin in order to facilitate bacterioscopic diagnosis of the disease. There are physiological, biological, thermal, mechanical and nutritional provocations.
A physiological provocation is menstruation, therefore, when using this method, smears from the urethra and cervical canal are recommended to be taken on the 2-4th day of menstruation.
Of the numerous methods of artificially activating the inflammatory process, the following are most often used:
1) intramuscular injection gonovaccines(500 million or more microbial bodies);
2) lubricating the mucous membrane of the cervical canal and urethra Lugol's solution on glycerin or silver nitrate solution(for the urethra - 0.5% solution, for the cervix - 2-3% solution);
3) physiotherapeutic procedures (inductothermy, zinc electrophoresis using a cervical or vaginal electrode, ultrasound, therapeutic mud).
Currently, pyrogenic drugs are widely used to provoke gonorrhea. (pyrogenal). After these provocation methods, it is necessary to take smears after 24, 48, 72 hours.
In a number of patients, in order to identify the latent form of gonorrhea, to determine the biological properties of the flora and determine sensitivity to antibiotics, as well as to identify tuberculosis bacilli when a specific inflammatory process in the genitals is suspected, it is used bacteriological examination by the culture method, i.e. sowing secretions from various parts of the reproductive system on artificial nutrient media. Material for bacteriological examination is taken with a sterile swab on a wire, which is slowly placed in a sterile tube and sent to the laboratory.
In clinical outpatient practice for the purpose of early diagnosis of genital cancer, it is widely used cytological method research. For cytological examination of the cervix, smears should be taken from the surface of the vaginal part and from the cervical canal. The material can be obtained using anatomical tweezers, a Volkmann spoon, a grooved probe or a special metal spatula with a notch at the end. Smears from the uterine cavity are obtained by aspiration with a syringe having a long tip (Brown syringe). The resulting smears from various parts of the reproductive system are applied to glass slides, fixed in a mixture of alcohol and ether, stained and examined under a microscope to identify atypical cellular complexes.
Functional diagnostic tests.
Tests evaluate the hormonal function of the ovaries. The nurse should be familiar with the most simple and accessible functional diagnostic tests.
Cervical mucus examination based on change physical and chemical properties mucus during the menstrual cycle. Its amount increases from 60-90 mg/day in the early follicular phase to 600-700 mg/day during the period of ovulation; By the same period, the activity of some mucus enzymes increases and its viscosity decreases. The “pupil” and “fern” phenomena are based on changes in the secretion and refractive power of cervical mucus.
Symptom (phenomenon) of “pupil” allows us to judge the production of estrogen by the ovaries. From the 8-9th day of the two-phase menstrual cycle, the external opening of the cervical canal begins to expand, reaching a maximum at the time of ovulation; glassy transparent mucus appears in it. When directed by a beam of light, the external pharynx with a protruding drop of mucus appears dark and resembles a pupil. In the second phase of the cycle, the external os of the cervix begins to gradually close, the amount of mucus decreases significantly, the symptom disappears by the 20-23rd day of the menstrual cycle. The test is not typical for cervical erosion, endocervicitis, or old cervical ruptures.
Fern symptom (arborization test) based on the ability of cervical mucus to form crystals when dried.
The material is taken from the cervical canal with anatomical tweezers at a depth of 0.5 cm; a drop of mucus is dried and the result is assessed under a microscope at low magnification.
The test is used to diagnose ovulation. The presence of the “fern” symptom throughout the entire menstrual cycle indicates high secretion of estrogen and the absence of the luteal phase; its lack of expression during the examination may indicate estrogen insufficiency.
Symptom of cervical mucus tension also allows us to judge the production of estrogen by the ovaries. Its maximum severity coincides with ovulation - mucus from the cervical canal, taken with tweezers, is stretched by the jaws by 10-12 cm.
Colpocytological examination- study of the cellular composition of vaginal smears, based on cyclic changes in the vaginal epithelium.
In vaginal smears, four types of cells are distinguished - basal, parabasal, intermediate and superficial:
I reaction: the smear consists of basal cells and leukocytes; the picture is typical for severe estrogen deficiency;
II reaction: the smear consists of parabasal, several basal and intermediate cells; the picture is characteristic of estrogen deficiency;
III reaction: in the smear there are mainly intermediate cells, there are single parabasal and superficial ones; the picture is characteristic of normal estrogen production.
IV reaction: superficial cells and a small amount of intermediate cells are detected in the smear; The picture is typical for high estrogen production.
The quantitative ratio of cells in a smear and morphological characteristics are the basis of hormonal cytological diagnostics. The material for research is taken from the lateral fornix of the upper third of the vagina (the most sensitive to hormonal effects), without rough manipulation, since the cells to be examined are those that have separated from the vaginal wall.
To interpret the test, the following indices are calculated:
- maturation index (MI) - percentage superficial, intermediate and parabasal cells. Written as three consecutive numbers, for example: 2/90/8;
- karyopyknotic index (KI, KPI)- percentage of superficial cells with a pyknotic nucleus to superficial cells with nuclei.
During the ovulation menstrual cycle, the following fluctuations in CI (CI) are observed: in the first phase 25-30%, during ovulation 60-80%, in the middle of the second phase 25-30%.
It is assumed that there are three options for the penetration of microbes from the lower parts of the genital tract to the upper: with Trichomonas, with sperm, and passive transport due to the suction effect of the abdominal cavity. Exacerbation of the chronic inflammatory process is often caused by such unfavorable factors as hypothermia or overheating of the body, excessive physical or mental stress, stressful situations, occupational exposure, as well as general diseases.
Clinical manifestations of pelvic inflammatory diseases and the tactics of therapeutic approaches to them depend not only on the nature of the infectious agent: the woman’s age and previous health status, possible invasive diagnostic, therapeutic and other interventions on the genital apparatus, but also on the location of the lesion.
Depending on the localization of the process, inflammation of the external genitalia (vulvitis, bartholinitis), vagina (colpitis), uterus (endocervicitis, cervicitis, cervical erosion, endometritis), uterine appendages (salpingoophoritis), pelvic tissue (parametritis), pelvic peritoneum (pelvioperitonitis) and diffuse inflammation of the peritoneum (peritonitis).
The most common symptoms of acute inflammation of the female genital organs are local pain, leucorrhoea, swelling of the affected organ, as well as often an increase in body temperature and a change in the blood picture characteristic of the inflammatory process (leukocytosis, increased ESR). Sometimes menstrual function is disrupted.
In subacute inflammation, the pain is moderate, the body temperature is not higher than subfebrile, and there are little or no changes in the blood picture. In chronic inflammation, the appearance of an acute process is regarded as an exacerbation.
In the chronic stage of the inflammatory process in the affected organ, changes in nerve receptors and capillaries, proliferation of connective tissue with the formation of adhesions, as well as changes in the general immunological reactivity of the body are observed.
Nonspecific inflammatory diseases female genital organs arise under the influence of the so-called pyogenic flora (staphylococci, coli and etc.).
Rarely, the cause of nonspecific inflammatory diseases may not be microbial, but mechanical, thermal and chemical agents. Usually the disease is preceded by some kind of surgical intervention (artificial abortion, diagnostic curettage of the mucous membrane of the uterine body, biopsy) as a result of which an entrance gate for infection is formed. Violation of hygiene of the genital organs and sexual life, inflammatory diseases urinary system and intestines are also a source of inflammatory diseases of the female genital organs.
Vulvitis- inflammation of the external genitalia. With this disease, patients complain of burning, pain, and often itching in the area of the labia and vaginal opening. When examining the external genitalia, hyperemia and swelling of the tissues, purulent discharge, and possible ulcerations are noted.
For successful treatment vulvitis, it is necessary to find out the reasons predisposing to this disease(ovarian hypofunction, diabetes mellitus, helminthiases, non-compliance with personal hygiene rules, masturbation, etc.), and eliminate them. Local treatment consists of hygienic treatment of the genitals with various disinfectant solutions(potassium permanganate in a ratio of 1:10,000, 2% boric acid solution, chamomile infusion, etc.) followed by lubrication with syntomycin liniment or streptocide emulsion, ointment with vitamins, estrogens. Sitz baths made from infusions of chamomile, potassium permanganate, St. John's wort, and string are also recommended.
Bartholinitis is inflammation of the large vestibular gland. It is characterized by sharp pain, swelling and infiltration in the labia majora area. During the purulent process, the temperature rises, the blood test shows leukocytosis, an increase in ESR.
Treatment. In the acute stage of the disease, the patient is prescribed bed rest, antibiotics, vitamins, place an ice pack on the area of the affected gland.
At purulent inflammation hospitalization and surgical treatment are required - opening of a purulent focus with subsequent introduction of turundum into its cavity with hypertonic 10% sodium chloride solution, and then with Cherry ointment. At the stage of resorption of the process, physiotherapeutic treatment sessions (UHF, ultrasound) are indicated.
In the area of the vulva, perineum, as well as the vagina and cervix, they sometimes develop genital warts. The cause of condylomas is considered to be a filterable virus. Secondary addition of pyogenic flora causes inflammation and necrosis of condylomas.
Treatment of condylomas consists of sprinkling them with resorcinol powder with boric acid, and in case of large quantities, removing them surgically or by electrocoagulation.
Colpitis is inflammation of the vagina. Signs of the disease are copious discharge(leucorrhoea), often pain in the vagina. The walls of the vagina are hyperemic, swollen, and sometimes pinpoint bright red rashes and purulent deposits are visible. With trichomonas colpitis, the discharge is purulent, yellow-green, foamy, and with thrush - in the form of white curdled masses.
Treatment should be comprehensive, taking into account the pathogen, microscopic and microbiological examination data. General anti-inflammatory treatment is carried out in combination with local use of disinfectants, antibacterial, anti-inflammatory agents. Treatment of recurrent colpitis is long-term, courses last 2-3 weeks. After use antibacterial drugs be sure to prescribe medications for recovery normal microflora vagina - lactobacterin, bifidumbacterin and dialact for local use.
In childhood and old age, simultaneous inflammation of the vagina and external genitalia is more often observed - vulvovaginitis. In girls, vulvovaginitis often develops when pinworms infect the rectum, with urinary tract disease, and also when foreign bodies enter the vagina. In these patients it is necessary to reverse Special attention to identify gonorrhea, which, as a rule, has a household route of infection.
The specifics of treatment for vulvovaginitis depend on the etiology of the disease.
Endocervicitis- inflammation of the mucous membrane of the cervical canal. The disease manifests itself as leucorrhoea and sometimes nagging pain in the sacral area. In the acute stage of inflammation, when examining the cervix with the help of mirrors, hyperemia around the external pharynx, mucopurulent or purulent discharge from the cervical canal. In the chronic course of the process, hyperemia is expressed insignificantly, the discharge from the cervical canal is mucous and cloudy. Long-term chronic course of endocervicitis leads to hypertrophy (thickening) of the cervix - cervicitis.
Treatment - comprehensive local and general with the use of antibacterial, anti-inflammatory, vitamin (A And E) and restorative drugs.
Cervical erosion is damage, a defect in the stratified squamous epithelium on the vaginal part of the cervix around the external os. Such erosion is usually called true. It is formed as a result of irritation of the cervix by pathological discharge from the cervical canal during endocervicitis. True erosion is bright red in color, irregular shape, bleeds easily when touched.
Stage true erosion does not last long (1-2 weeks), its healing soon begins. In the first stage of healing (pseudo-erosion), the defect of the stratified squamous epithelium is replaced by a cylindrical one, spreading from the cervical canal. This epithelium is brighter in color compared to stratified squamous epithelium, so the surface of the erosion remains bright red. Pseudo-erosion can exist for many months and even years if left untreated.
When the inflammatory process subsides spontaneously or under the influence of treatment, stage II of erosion healing occurs, in which the stratified squamous epithelium from the edges begins to displace or cover the columnar epithelium. Often, small (Nabothian) cysts remain at the site of former erosion, which are the result of blockage of the excretory ducts of the erosive glands. Erosions are often formed when the mucous membrane of the cervical canal is everted (ectropion) at the site of former ruptures - eroded ectropion.
It is now known that cervical erosion can be not only a consequence of inflammation, but also the result of congenital and dystrophic changes in its epithelium, as well as hormonal disorders in a woman’s body. In the presence of erosion, a woman is bothered by pathological discharge, usually of a mucopurulent nature, sometimes contact bloody discharge and nagging pain in the sacral area.
Treatment of chronic cervicitis in combination with cervical erosion is long-term. Initially, conservative treatment is carried out (hygienic douching, medicinal baths, tampons or balls with antimicrobial drugs, rosehip oil, sea buckthorn, fish oil). The lack of effect from the therapy is an indication for a biopsy of cervical erosion (after colposcopy), followed by electrocoagulation, cryotherapy, and laser therapy. With eroded ectropion, they often produce plastic surgery on the cervix. Endometritis- inflammation of the uterine mucosa.
Sometimes the inflammatory process takes over and muscle layer uterus. Endometritis is manifested by cloudy, sometimes purulent discharge from the genital tract, aching pain in the lower abdomen and in the sacral area. Acute endometritis is characterized by a general reaction of the body to the inflammatory process: increased body temperature, tachycardia, chills. The main clinical sign of chronic endometritis is menstrual dysfunction, mainly in the form of bleeding. In modern conditions, endometritis can occur in an erased form from the very beginning.
Salpingo-oophoritis (adnexitis)- inflammation of the uterine appendages. The disease in the acute stage is characterized by intense pain in the lower abdomen, more pronounced on the affected side. Often salpingoophoritis is bilateral and is combined with inflammation of the uterus. Body temperature is usually elevated, and with purulent inflammation it can be high and accompanied by chills. As the inflammatory process increases, a purulent saccular tumor sometimes develops in the area of the uterine appendages - a tubo-ovarian tumor.
Inflammatory diseases of the uterine appendages cause infertility, ectopic pregnancy, menstrual dysfunction, etc.
Parametritis- inflammation of the periuterine tissue. This disease is characterized by pain in the lower abdomen with irradiation to the legs and sacral area, difficulty urinating and defecating due to severe pain, deterioration in general condition, and increased body temperature. When the parametric infiltrate suppurates, its contents may leak into the bladder or rectum.
Pelvioperitonitis- inflammation of the pelvic peritoneum, most often resulting from the spread of infection into the abdominal cavity from the infected uterus, tubes and ovaries. With this disease, severe pain in the lower abdomen, deterioration of general condition, and high temperature are noted. The disease may be accompanied by vomiting, retention of stool and gas, and intoxication symptoms: rapid pulse, decreased blood pressure, and a feeling of dry mouth. When examining the patient, symptoms of peritoneal irritation are evident in the lower parts of the abdomen.
Peritonitis- diffuse inflammation of the peritoneum, resulting from the progression of purulent pelvioperitonitis or rupture purulent formation uterine appendages. The disease is characterized by an increase in intoxication, an increase in body temperature to high numbers, and signs of irritation of the peritoneum, expressed in all parts of the abdomen. The development of diffuse peritonitis requires emergency surgical intervention.
Treatment of patients suffering from acute, subacute inflammatory process and exacerbation of chronic inflammatory process of the uterus, appendages and surrounding tissues is carried out in a hospital setting. Treatment of these diseases is complex, carried out according to uniform principles, depends on the stage of the process and includes: antibacterial, detoxification, restorative, sedative, desensitizing, symptomatic therapy, physiotherapy, and, if indicated, surgical treatment.
The choice of antibiotics is determined by the microflora that caused the disease and its sensitivity to them. More often, a combination of antibiotics and drugs that act on anaerobic bacteria is prescribed. (metronidazole, clindamycin, etc.), as well as with nitrofurans. In the case of tubo-ovarian formations or the development of peritonitis, surgical treatment is necessary.
In chronic stages of the disease, vitamin therapy with physiotherapy is used, spa treatment(balneo- and mud therapy).
Specific inflammatory diseases female genital organs develop as a result specific infection(gonorrhea, tuberculosis, trichomoniasis, chlamydia, AIDS, etc.).
Gonorrhea is a specific infectious disease caused by Neisser's gonococcus. Gonorrhea is usually transmitted through sexual contact, and less commonly (in children) through household transmission. The incubation period ranges from 3 to 6 days.
Gonococcus infects mucous membranes covered with cylindrical epithelium, therefore, when infected, the primary foci of the disease are the mucous membranes of the cervical canal, the urethra with paraurethral ducts and the excretory ducts of the large vestibular glands. The pathological process in the area of primary lesions is usually called gonorrhea of the lower female genital organs.
The spread of infection in gonorrhea occurs in an ascending way through the mucous membranes, or intracanalicularly. As a result of the penetration of gonococcus beyond the internal os of the cervix, gonorrhea of the upper genital organs, or ascending gonorrhea, develops. This affects the endometrium, fallopian tubes, ovaries and pelvic peritoneum. Ulcers often form fallopian tubes(pyosalpinxes) and ovaries (pyovariums).
The occurrence of ascending gonorrhea is facilitated by menstruation, abortion, childbirth, diagnostic curettage of the mucous membrane of the uterine body, and poor sexual hygiene.
According to the clinical course, fresh (up to 2 months from the moment of illness) and chronic gonorrhea are distinguished. There are acute, subacute and torpid (erased) forms of fresh gonorrhea. In recent years, cases of torpid diseases have become more frequent. In addition to the listed forms, there is latent gonorrhea. With this form, there are no symptoms of the disease, gonococci are not detected in smears, and patients are an undoubted source of infection. In the torpid form of gonorrhea, in contrast to the latent form, gonococci are found in smears.
The clinical picture of acute gonorrhea of the lower genital organs is manifested by profuse purulent leucorrhoea and frequent painful urination. During a gynecological examination of the patient, hyperemia in the area of the external opening is noted. urethra and external os of the cervix, mucopurulent discharge from the cervical canal.
The torpid form of gonorrhea occurs without pronounced clinical symptoms, so the patient may not see a doctor and be a source of infection for a long time.
Ascending gonorrhea is characterized by an acute onset, severe general intoxication and rapid reverse development process after prescribing antibacterial therapy. In the torpid form of ascending gonorrhea, the disease proceeds sluggishly, accompanied by unexpressed aching pain in the lower abdomen.
Gonorrhea of the upper genital organs involving the uterine appendages is most often bilateral and leads to infertility as a result of obstruction of the fallopian tubes.
Diagnosis of gonorrhea is based on identifying gonococcus in the urethra, cervical canal, and sometimes in discharge from the vestibular glands and rectum (bacterioscopic and bacteriological studies). With torpid and chronic course gonorrhea, to detect the pathogen, provocation methods are used, causing an exacerbation of the process.
Treatment of patients suffering from gonorrhea of the lower genital organs is carried out in regional venereal dispensaries, where a notification is sent and a woman is referred after gonococcus is detected in her smears. Patients suffering from ascending gonorrhea are usually treated in a gynecological hospital. The principles of treatment for patients with gonorrhea do not differ from those for patients with an inflammatory process of septic etiology. General therapy (antibacterial, desensitizing, detoxification, etc.) in the subacute and chronic stages is combined with local treatment of the lesions.
For this purpose it is used 1-3% silver nitrate solution, 1-3% protargol solution, 5% collargol solution. IN venereal dispensary In addition to treatment, the patient is confronted (identifying the source of infection). After treatment is completed, the patient is carefully examined to determine whether she is cured. For this purpose, smears are taken from the patient during three menstrual cycles on the days of menstruation (on the 2-4th day). If during this time no gonococcus is detected in smears, then the patient is considered cured of gonorrhea (cure criterion).
Trichomoniasis- a specific infectious disease caused by Trichomonas vaginalis. Trichomoniasis is usually transmitted through sexual contact. Extrasexual transmission is rare. The incubation period is 5-15 days.
The clinical picture of the disease is characterized by symptoms of colpitis. Sometimes the urethra, bladder and rectum are affected. Patients usually complain of profuse leucorrhoea, itching in the area of the external genitalia and vagina. The walls of the vagina are hyperemic, swollen, and there is abundant yellow-green foamy discharge. When the clinical symptoms of trichomoniasis are mild, patients do not always consult a doctor in a timely manner. In such patients, the disease is characterized by a protracted course and a tendency to relapse.
Recognition of trichomoniasis is carried out by microscopic examination of discharge from the vagina, cervix and urethra.
Treatment of trichomoniasis is carried out on an outpatient basis with special oral bactericidal drugs: trichopolum, flagyl, trichomonacid, fasigin. Local treatment of trichomoniasis consists of daily treatment of the vagina with disinfectant solutions and injection into the vagina metronidazole in the form of candles, Klion-D in the form of vaginal tablets. Simultaneously with the patient according to the same scheme oral medications her partner must be treated.
Cure criteria: during three menstrual cycles, smears are taken on the days of menstruation. If Trichomonas are not detected, then the patient is considered cured of trichomoniasis.
Tuberculosis genitals women, caused by Mycobacterium tuberculosis, is a secondary disease. The history of a patient with genital tuberculosis usually indicates tuberculosis of the lungs or other organs in the past.
The fallopian tubes and uterus are most often affected, less commonly the ovaries and extremely rarely the vagina and external genitalia. Typically, the disease manifests itself during the formation of menstrual function and the beginning of sexual activity. It proceeds sluggishly, without pronounced pain syndrome, with low-grade body temperature, which does not decrease as a result of nonspecific anti-inflammatory therapy. Menstrual dysfunction is often observed in the form of bleeding at the onset of the disease and scanty menstruation until its complete cessation during a prolonged process. A characteristic symptom of genital tuberculosis is primary infertility.
If genital tuberculosis is suspected, the patient should be referred for consultation to an anti-tuberculosis dispensary, where she undergoes special examination and treatment to confirm the diagnosis.
Treatment, as well as diagnosis, should be carried out in specialized TB institutions.
Candidiasis - an infectious disease of the vagina that spreads to the cervix and often to the vulva. The causative agent is yeast-like fungi, most often of the genus Candida. The occurrence of candidiasis colpitis is promoted by diseases that reduce the body's defenses (diabetes mellitus, tuberculosis, diseases of the gastrointestinal tract, etc.), as well as long-term use of antibiotics and hormonal contraceptives, leading to dysbacteriosis.
Candidiasis is especially often detected in pregnant women, which is due to changes in the endocrine and other body systems that occur during pregnancy. Patients complain of leucorrhoea, itching and burning in the vulva area. Leucorrhoea can be of a different nature, most often containing an admixture of cheesy-crumbly inclusions. Upon examination, grayish-white deposits of a cheesy nature are noted on the affected mucous membranes of the genital organs. After removing the plaque, a brightly hyperemic mucous membrane is revealed.
The course of candidiasis can be long, lasting for years with periodic relapses, despite treatment, which is especially typical in the presence of other foci of candidiasis in the body.
Clarification of the diagnosis is based on the detection of the pathogen in smears taken from the affected areas.
Treatment is complex, directed directly against the pathogen and including treatment of concomitant diseases. A combination of oral administration is required antifungal drugs (nystatin, nizoral, diflucan) with local treatment. Used intravaginally ginopevaril, gynotravogen, miconazole, nystatin in candles, cloprimazole, pimafucin V vaginal tablets and cream, tampons soaked 10-20% solution of borax in glycerin, etc. Treatment courses also include vitamins, sedatives, restoratives and desensitizing agents.
Chlamydia caused by chlamydia (an intermediate form between bacteria and viruses), transmitted sexually, characterized by a long course, insufficient expression clinical signs, a tendency to relapse.
Chlamydia can coexist with mycoplasmas, gonococci and other bacteria. The incubation period lasts 20-30 days. The primary focus of infection is usually located in the mucous membrane of the cervix, characterized by purulent (seropurulent) discharge from the cervical canal and hyperemia around the external os. It is possible to develop chlamydial urethritis, which is accompanied by dysuric symptoms or occurs against a background of mild symptoms.
Chlamydial infection affects almost all parts of a woman’s genital organs, causing the development of bartholinitis, cervicitis, pseudo-erosion on the cervix, endometritis, salpingitis, and pelvioperitonitis. As a result, violations of the basic functions of the reproductive system occur, often leading to infertility.
Chlamydia in pregnant women deserves special attention, since they have a risk of infection during childbirth (chlamydial conjunctivitis, pneumonia, etc.).
Clinical manifestations of chlamydia are nonspecific and, as a rule, differ little from signs of diseases caused by other microorganisms.
Diagnostic methods can be divided into two groups
.
The first group includes the detection of a pathogen (or its antigen) by immunofluorescence and enzyme immunoassay methods in the affected tissue. The most accessible material is smears from the cervical canal, obtained by superficial scraping. The second diagnostic method is based on determining antibodies against chlamydia in the patient’s blood serum.
Currently, the most specific method has been developed - determination of pathogen DNA in pathological material (DNA diagnostics).
The success of treatment depends on early diagnosis and timely treatment, simultaneous examination and treatment of the husband (sexual partner), cessation of sexual activity until complete recovery, prohibition of the use of alcohol and spicy food. The basis of therapy is antibiotics: tetracyclines (mainly doxycycline), macrolides ( erythromycin, sumamed, rulid), fluoroquinolones ( abaktal, tsiprobay, tsifran). It is necessary to simultaneously prevent candidiasis nystatin, nizoral and etc.
Viral diseases are among the common infections of the genital organs and can be caused by various viruses. Some viruses (for example, cytomegalovirus, hepatitis B virus) do not cause noticeable changes in the genitals, but during pregnancy they pose a real threat to the fetus. The most clinically pronounced diseases of the genital organs are caused by the herpes simplex virus and papillomavirus.
Herpes simplex virus is the causative agent of herpetic diseases of the genital organs, is transmitted sexually and persists for life in regional lymph nodes and nerve ganglia, periodically leading to relapses of infection. The main reservoir of the virus in men is genitourinary tract, in women - the cervical canal.
Clinical symptoms of genital herpes usually appear within 3-7 days incubation period. Local manifestations (erythema, vesicles, ulcers) occur on the mucous membranes of the vulva, vagina, cervix, sometimes in the urethra and perineum. They are accompanied by itching, burning, pain, as well as general malaise, headache, low-grade fever, etc.
The severity of the clinical picture, the frequency of relapses and the duration of remissions vary individually within wide limits. The occurrence of relapses is facilitated by such factors as stress, overwork, hypothermia, and the addition of other diseases. In case of defeat upper sections reproductive system, infertility is possible. The disease is sometimes asymptomatic. Genital herpes can have adverse consequences during pregnancy: the fetus can become infected and develop developmental abnormalities.
For diagnosis, various complex methods (electron microscopic, etc.) are used to detect the virus in the discharge from the affected organs or antibodies to it in the patient’s blood serum.
Antiviral drugs are used for treatment - Zovirax (Virolex, Acyclovir), Famvir, Alpizarin, Helepin and others, which temporarily stop the spread of the virus, reduce the frequency of relapses, but do not cure the disease. Antiviral drugs in the form of ointment ( Zovirax, Bonafton, Gossypol, Triapten, etc.) used topically when the first symptoms appear herpetic infection. To prevent and treat relapses of the disease, immunocorrective therapy is prescribed.
Broadcast human papillomavirus infection occurs only sexually. This disease is also known as condylomas. The most common are pointed condylomas, located mainly in the area of the labia majora and minora, less often in the vagina, on the cervix and in the perineum. Possible proliferation of condylomas, especially during pregnancy.
Treatment consists of treating condylomas feresol, coidilin (0.5% podophyllotoxin solution), and if there is no effect - removal using cryodestruction, carbon dioxide laser, electrocoagulation. Bacterial vaginosis- a disease (previously called gardnerellosis), in which there is a disruption of the normal microflora of the vagina (vaginal dysbiosis) with a predominance of opportunistic pathogens: gardnerella, bacteroides, mycoplasmas and other microorganisms. The disease is asymptomatic; leukocytes and pathogenic pathogens are not detected in the vaginal secretion. Patients complain of profuse leucorrhoea with an unpleasant smell of rotten fish.
Diagnostic signs are an increase in the pH of the vaginal environment more than 4.5 (normally 3.8-4.2); presence of key cells on vaginal smear microscopy, positive amine test (when added to the vaginal contents 10% potassium hydroxide solution a sharp, specific smell of fish is detected).
Treatment is aimed at restoring normal vaginal microflora. Desensitizing and immunocorrective therapy is carried out. At the first stage of treatment, drugs are applied topically metronidazole(in gel, suppositories, tablets) or vaginal form clindamycin(dalacina-C). Oral metronidazole or clindamycin can be used at this stage. At the second stage, biological products (eubiotics) are prescribed intravaginally: lactobacterin, bifidumbacterin, acylact.
Infectious diseases of the female genital organs that are sexually transmitted (such as syphilis, gonorrhea, trichomoniasis, chlamydia, ureaplasmosis, candidiasis, genital herpes, etc.) are combined into general group under a single name: sexually transmitted diseases (STDs).
HIV infection is a disease caused by the human immunodeficiency virus (HIV), which persists for a long time in lymphocytes, macrophages, and nerve tissue cells. As a result of exposure to the virus, slowly progressive damage to the immune and nervous systems of the body develops, manifested by secondary infections, tumors, subacute encephalitis and other pathological processes leading to the death of the patient. HIV infection occurs through several stages, the last of which is referred to as “HIV syndrome.”
FULL NAME.
Age: 67 years old
Pensioner, disabled group 1
Place of residence: Moscow
Complaints
The patient complains of shortness of breath with slight physical exertion (when climbing 1.5 floors) and at rest, worsening in a horizontal position, shortness of breath turning into suffocation, short-term pain behind the sternum, squeezing and pressing in nature, radiating to the area of the left shoulder blade, which is relieved by nitroglycerin in for 5 minutes, palpitations, increasing in a horizontal position, temperature rise to 38 0 C, dizziness, tinnitus, severe weakness, increased fatigue.
Family history
My grandmother on my father’s side suffered from rheumatism.
My father died at the age of 71 from laryngeal cancer.
The mother died at the age of 71 from stroke.
The sister (the eldest) suffered from a heart defect (the diagnosis was the same as that of the patient). She died of liver cancer at the age of 57.
As a child, my daughter often suffered from sore throat. Diagnosed at age 5
mitral valve disease with predominant stenosis. In the same year she was in Morozov Hospital where a tonsillectomy was performed. For the next 2 years she was in sanatorium-resort treatment. At the age of 7 the diagnosis was removed.
Anamnesis of life
The patient was born at term, the second child in the family, parents' age: mother - 24 years, father - 27 years. In the 40s, during the war, she was forced to hide in bomb shelters (trenches), where she was exposed to hypothermia. She did not lag behind in physical and mental development. Received higher education, worked for 30 years in chemical production related to the application of coatings on aircraft (constant contact with acetone, toluene, epoxy resins). For the last 4 years I have worked with a gardening partnership, where I was constantly exposed to emotional stress, and therefore left my job. Currently not working (retired), married, has a daughter, good housing and communal conditions: she lives in an apartment with heating, on the 5th floor, the building has an elevator. He follows a diet (he limits himself in the consumption of salty, spicy, fried foods), tries to eat more vegetables and fruits. Has a disability
I group since 1998 for the main disease.
Does not smoke, does not abuse alcohol, coffee, or tea.
Gynecological history
Menstruation began at the age of 11, regular, duration of the menstrual cycle 28 days, duration of menstrual bleeding 6 days, painless.
2 pregnancies, 1 childbirth, 1 abortion.
Pregnancy (24 years old) proceeded without complications (under constant supervision of the attending physician), childbirth - without complications.
At the age of 27, he underwent surgery to remove a left ovarian cyst.
Menopause from age 46.
Chapter 39
GYNECOLOGY
Anatomy
External genitalia (vulva)
The labia majora form the skin borders on the sides of the vulva and are analogous to the scrotum in men. In front they come into contact with the anterior eminence (pubic symphysis, eminence of Venus), in the back - with structures related to the posterior commissure. Medial to the labia majora are the labia minora, covered laterally by hair-free skin, and medially by the vaginal mucosa. The anterior junction of the labia minora forms the foreskin of the clitoris, the posterior junction forms the frenulum of the labia. Pelvic floor muscles (pelvic diaphragm)
Muscles, elevating the anus, form the muscular pelvic floor and include mm. pubococcygeus, puborectalis, iliococcygeus And coccygeus. Distal to the levator anus muscle are the superficial muscles that make up the urogenital diaphragm. Lateral to these muscles are t. ischiocavernosus. Mm. bulbocavernosus And transverse the perineal muscles, intertwining medially, originate from the pubic symphysis. Internal genitalia
The muscles on the pelvic side are represented by mm. iliacus, psoas And obturator internus. The blood supply comes from the internal iliac arteries, except for the middle sacral artery. The internal iliac and hypogastric arteries divide into anterior and posterior branches. The anterior branch of the hypogastric artery gives rise to the obturator, uterine, superior and middle cystic arteries. Innervation is provided by the sciatic, obturator and femoral nerves. Gynecological history
The gynecological history should include the patient's age, date of last menstruation, number of pregnancies, births and abortions, general state health and last contraceptive method used. Physical examination
A gynecological examination includes examination of the mammary glands, abdomen and pelvis, external genitalia with recording of the results, examination of the vagina in the speculum and taking a smear from the cervical canal for cytological examination. After removing the speculum, a bimanual pelvic examination is performed. Then - rectovaginal examination. Diagnostic tests
Cytological examination of the cervical canal
Performed from the age of 18 or earlier if the patient is sexually active. Most women and patients who have had a total hysterectomy for a cervical tumor should have this procedure done annually. For pathologies not associated with neoplasms of the cervical canal, the vaginal vault is examined cytologically every 3-5 years. The classification of cervical pathology is presented in table. 39.1. Atypical smears or smears with signs of severe inflammation are repeated after 3 months. If the atypical picture in the smears persists, colposcopy is indicated, which makes it possible to distinguish dysplasia from neoplasia. Tissue biopsy
A tissue biopsy for suspected lesions of the vulva, vagina, cervix and uterus should be carried out in a specialized institution. A vulvar biopsy is done after infiltrating the biopsy area with a small amount of 1% lidocaine solution using an appropriate (27) gauge needle. In contrast, ectocervical biopsy does not require anesthesia. Endometrial biopsy should be performed only in an appropriate medical institution; before the procedure, it is necessary to ensure that the patient is not pregnant. Examination of vaginal discharge
Pathological vaginal discharge is subject to examination. Normal vaginal pH is 3.8-4.4; at a pH of 4.9 or more, examination for bacterial and protozoal infections is indicated. The wet native preparation is placed on the mounting table of the microscope in a small amount of saline and under a coverslip. Motile trichomonas are characteristic of vaginal trichomoniasis, “key cells” are characteristic of bacterial vaginitis, the presence of leukocytes indicates various inflammatory diseases of the vagina, cervix and urinary tract, such as gonorrhea, chlamydia. A 10% potassium hydroxide solution is added to the sample and vaginal material for re-examination. Potassium hydroxide lyses cellular material and makes it possible to see the mycelium characteristic of candidiasis vaginitis. Table 39.1. Classification for cytological examination of the cervix (USA)
MATCHING PATTERN Satisfactory for research
Satisfactory for research, but limited... (specificity)
Unsatisfactory... (specificity)
Within normal limits
Benign cell changes (see descriptive diagnosis)
Abnormal epithelial cells (see descriptive diagnosis)
DESCRIPTIVE DIAGNOSIS OF BENIGN CELL CHANGES Trichomoniasis (Trichomonas vaginalis)
Fungal infections
Predominance of coccal flora
Contains actinomycetes (Actinomyces sp.)
Contains herpes simplex virus
REACTIVE CHANGES Changes caused by inflammation
Atrophy combined with inflammation
Irradiation
Intrauterine contraception
EPITHELIAL CELLS, ANOMALIES, SQUAMOUS CELLS Atypical squamous cells, poorly differentiated
Squamous intraepithelial cell damage in the early stages of development, including human papillomavirus
Significant stage of development of squamous intraepithelial damage, including moderate and severe dysplasia, carcinoma in situ
Squamous cell carcinoma
Glandular cells Endometrial cells, cytologically benign in postmenopause Atypical glandular cells, poorly differentiated
Endocervical adenocarcinoma
Endometrial adenocarcinoma
Ectopic adenocarcinoma
Nonspecific adenocarcinoma
OTHER MALIGNANT NEOPLASMS (specificity) HORMONAL EXAMINATION (only a vaginal smear is used)
Hormonal fingerprint smear consistent with age and history
Hormonal smear fingerprint that does not correspond to age and medical history
Hormonal examination is impossible due to... (reasons)
Cultivation of microorganisms
Suspicion of gonorrhea arises in the presence of gram-negative intracellular diplococci found in the vaginal mucus with Gram staining. When cultured with gonococci, gonorrhea is confirmed; pathogen, cultivated on “chocolate” agar. Pregnancy tests
Determined increased amount p-subunits of human chorionic gonadotropin in urine. Serial determination of hormone levels is used in the treatment of threatened miscarriage, ectopic pregnancy, or trophoblastic diseases. Pathological bleeding
The menstrual cycle varies from 21 to 45 days with bleeding duration from 1 to 7 days. Bleeding in combination with pregnancy
Bleeding can occur in 25% of cases during a normal pregnancy, but should be considered as an impending miscarriage until the bleeding stops. In case of threatened miscarriage, the cervical The third canal is closed and the uterus is assessed from the perspective of anamnesis and gestational age. Abortion in progress is diagnosed when the cervical canal is open and fetal tissue appears in the canal. Abortion is incomplete after partial expulsion of the fertilized egg. In case of incomplete abortion and abortion, curettage is performed. An ectopic pregnancy should be considered in any patient with a positive pregnancy test, pelvic pain, and abnormal uterine bleeding. Trophoblastic diseases may also cause abnormal bleeding, combined with a positive pregnancy test. Chorioadenoma (hydatidiform mole) is suspected due to excessive enlargement of the uterus (according to a history of pregnancy) and the presence of grape-like tissue in the vagina. Ultrasound is used for diagnosis. Dysfunctional uterine bleeding
It is characterized by irregular menstruation with rare long intervals of amenorrhea. As a rule, the cause is secondary ovarian failure. During the examination, a pregnancy test is necessary. The study reveals non-secreting or proliferative endometrium. If the bleeding is severe, curettage is required, but in most cases cyclic treatment with estrogen and progesterone is prescribed. Secondary bleeding from neoplasms
Tumors of a benign and malignant nature affect the genital organs from the vulva to the ovaries and can cause abnormal bleeding. Dysfunctional bleeding in the group of patients of reproductive age is most often caused by leiomyoma (fibroma). Ultrasound of the pelvis and other methods of examining this area can make a diagnosis. Bleedings combined with tumors of the fallopian tubes and ovaries are few in number; a tumor formation in the pelvis is almost always palpable. Bleeding not related to the genital area
Genital bleeding can be combined with secondary coagulopathy when using systemic anticoagulants, causing abnormal clot formation and hemostasis disorders. Pain
Pain combined with menstruation is defined as dysmenorrhea. Pain without a specific pathology is interpreted as primary dysmenorrhea. Secondary is combined with endometriosis, stenosis of the cervical canal and inflammation in the pelvis.
Acute pain in the pelvis occurs during an uncontrolled pregnancy, benign or malignant tumors, incomplete miscarriage or non-gynecological diseases.
Pregnancy pathologies include threatened miscarriage, ongoing abortion, and ectopic pregnancy.
Acute pain in the ovary is associated with the destruction of fibroids, torsion of an ovarian cyst or its tumor. Spontaneous rupture of an ovarian cyst is accompanied by very severe pain.
Secondary pain in inflammatory diseases is combined with fever and other manifestations of infection. The possibility of a non-gynecological disease should always be taken into account. Appendicitis and other acute pathology gastrointestinal tract can cause pain in the pelvis and abdominal cavity.
An accurate diagnosis is not always possible during the examination, so laparoscopy is used. Neoplasm in the pelvis
In women of reproductive age, pregnancy should always be assumed when the uterus is enlarged. Ovarian enlargement occurs during ovulation and hemorrhage in the corpus luteum, which is palpable quite early and in some cases exists for several weeks. Abdominal and vaginal ultrasonography are useful. An enlarged uterus may be associated with pregnancy, fibroids, adenoid fibroids, or a malignant tumor such as endometrial cancer or sarcoma. Ovarian enlargement is possible with endometriosis, ectopic pregnancy, tubo-ovarian abscess or benign (malignant) tumor. Infections
Fungal infection
The most common cause of genital itching may be fungi of the genus Candida. Itching is more common when sugar diabetes, pregnancy or antibiotic use. Diagnosis is made by examining vaginal secretions and being treated local application of any drug from the imidazole group. Pinworms are more common in little girls. Diagnosis is made by detection of adult worms or identification of eggs by microscopic examination of material from the perianal folds collected on an adhesive tape. Trichomonas vaginalis - common cause of infection in the vagina: h Le- reading: Metronidazole 250 mg 3 times a day for 7 days. G The skin of the genital organs is often affected pubic lice and itching. Treatment consists of using ointments according to the Kwell method. Gardenerellosis - the most common pathology caused by a pathogenic bacterium Gardenerella vaginalis. Vaginal discharge is scanty, gray-green in color with an unpleasant “fishy” odor. Diagnosis is made by detecting “clue cells” treatment carried out with metronidazole 500 mg per os every 12 hours. Viral infections
Papillomavirus(human papillomavirus) causes genital warts. They consist of a single growing formation similar to a tubercle. Diagnosed by biopsy. IN treatment use cauterizing drugs, laser, cryo- or electrocautery. Simple herpes manifested by the presence of painful blisters followed by ulceration. Initially, the infection is widespread; culturing the pathogen confirms the diagnosis. The attack can be interrupted and the interval between attacks lengthens when using acyclovir (Zovirax). The drug is prescribed per os no 200 mg 5 times a day. For patients with vulvar or vaginal ulceration as a result of a herpes infection, delivery by cesarean section is recommended. Molluscum contagiosum causes a group of itchy nodules with an umbilical-shaped depression in the center. Treatment consists of removal with a cautery or curettage. Pelvic inflammatory diseases
In the United States, approximately 1.5 million cases of pelvic inflammatory disease occur annually, the prevalence of which is limited to sexually active women. Risk factors include: age under 20 years, having a large number of sexual partners, infertility and previous infections. The most common microbes are gonococcus And chlamydia. Classic symptoms include fever, pain in the lower abdomen with tenderness on examination of the pelvis, and purulent vaginal discharge. Differential diagnosis includes acute appendicitis, ectopic pregnancy, gastrointestinal obstruction or perforation, and urolithiasis. The correct diagnosis is made on the basis of laparoscopy, ultrasonography and CT examination of the pelvis. Treatment. Patients with peritonitis, high fever, or suspected tubo-ovarian abscess receive intravenous antibiotics. The CDC recommends cefoxitin 2 g intramuscularly with probenecid per os or ceftriazone 250 mg intramuscularly, or an equivalent cephalosporin with doxycycline 100 mg per os twice daily for 10 to 14 days. Treatment of patients in the hospital includes cefoxitin 2 g intravenously every 6 hours in combination with a large dose of gentamicin (2 mg/kg) intravenously, followed by a dose of 1.5 mg/kg every 8 hours. Doxycycline 100 mg orally twice daily for 10-14 days after the patient is discharged from the hospital. Another treatment option is clindamycin 900 mg IV every 8 hours with a high dose of gentamicin (2 mg/kg) IV, then 1.5 mg/kg IV every 8 hours. Patients discharged from the hospital receive doxycycline 100 mg twice daily per os. within 10-14 days. Surgical treatment. Used for intraperitoneal rupture of tubo-ovarian abscess, abscess and chronic pain in the small pelvis. For some period of time, in case of diffuse inflammation, hysterectomy with bilateral salpingo-oophorectomy was considered the operation of choice. Now, mainly in young women with unrealized reproductive function, a less radical operation is used. Endometriosis
Endometriosis accounts for approximately 20% of all laparotomies in women of reproductive age. Most common between 30 and 40 years of age. The exact cause of the disease is unknown. There is a theory that the onset is related to degenerating menstruation. The pathological appearance, often described as a "powder of fire" appearance, is bluish or black in color. The disease often affects the ovaries, and the process is bilateral. Other organs affected are the uterosacral ligaments, the abdominal surface of the deep pelvis, the fallopian tubes and the rectosigmoid region. Many patients have no clinical symptoms, even with a significant spread of the process, while others suffer from severe pain, partial dysmenorrhea and sexual dysfunction. Often accompanied by infertility and dysfunctional bleeding. The detection of neoplasms in the pelvis and painful nodes of the uterosacral ligament gives serious grounds to suspect endometriosis. Although Endometriosis may be suspected at the onset of clinical manifestations, biopsy and imaging of the pathology, preferably by laparoscopy, is necessary for accurate diagnosis. Treatment. The choice of treatment includes eliminating the disease conservatively or surgically. Cyclic oral contraceptives and conventional analgesics are often recommended for asymptomatic patients with minimal forms of endometriosis. It is considered useful to use the pseudopregnancy state for the use of high-dose oral contraceptives. Danazol (danocrine) is a weak oral androgen. The recommended dose is 400-800 mg daily for 6 months or longer. In recent years, gonadotropin-releasing hormone agonists have been used to simulate the state of pseudomenopause. Both danazol and gonadotropin-releasing hormone agonists are used in pre- and postoperative therapy in conjunction with surgical treatment. Conservative surgery involves excision of all visible and accessible endometriosis nodes while preserving the patient's reproductive capabilities. Ovarian endometriosis, known as “chocolate cysts,” is treated with organ-sparing resection. The pregnancy rate after conservative surgery approaches 50%. If extirpation is indicated, it is important to remove all ovarian tissue to prevent stimulation of residual endometriosis. Total hysterectomy with bilateral salpingo-oophorectomy and hormone replacement therapy for re-treatment if the first operation is ineffective, it is rarely used. Ectopic pregnancy
Over the past 20 years, the number of ectopic pregnancies has increased significantly. Due to improved diagnostic methods and treatment approaches, maternal mortality has decreased. For women in the last 10 years of their reproductive period, the risk is more than 3 times higher than for women 16-26 years old. The history contains indications of salpingitis. Clinically detect pain, often in combination with irregular uterine bleeding, tenderness of the uterine appendages, palpable in 50% of cases, and pain in the pelvis. For diagnosis, the most important laboratory test is a test to determine the β-subunits of human chorionic gonadotropin. Ultrasonography of the pelvis with a vaginal probe allows you to accurately differentiate between uterine and ectopic pregnancies. In emergency cases, the level of P-subunits of human chorionic gonadotropin is determined every 24-48 hours. In a normal pregnancy in the early stages, the level of the hormone doubles every two days. A vaginal test makes it possible to clinically determine pregnancy in the uterus or tube when the hormone level increases by more than 1000 times. In women who do not want to continue pregnancy, curettage of the uterus with examination of tissue can be diagnostic. If fetal tissue is absent, diagnostic laparoscopy is indicated. Laparoscopy. One of the most important methods of diagnosis and surgical treatment, used over the past decades. Partial salpingectomy is now performed laparoscopically. For a significant period of ectopic pregnancy, total salpingectomy or linear salpingotomy is used. Intra-abdominal operations. The same treatment is optimal for patients whose condition requires laparotomy. Defects of the pelvic support (bottom)
Defects of the pelvic support (fundus) include uterine prolapse, cysto-, recto- and enteroceles, urethral avulsion, and vaginal prolapse after hysterectomy. This pathology occurs due to birth injuries; conditions accompanied by increased intra-abdominal pressure, obesity, decreased estrogen levels, secondary tissue weakness due to hereditary factors or associated with malnutrition. Uterine prolapse
Uterine prolapse is the descent of its appendages onto the pelvic bones and vagina. If the cervix protrudes at the entrance to the vagina, then this is partial prolapse. If the uterus completely prolapses, then it is total. Cystocele and rectocele
The condition is caused by a hernial protrusion of the bladder and rectum into the vagina through a wide opening. Enterocele
Hernial protrusion of intra-abdominal organs into the vaginal vault. Most often occurs after hysterectomy. Enteroceles are often misdiagnosed as rectoceles. Urethral avulsion
At one time, avulsion of the urethra was called a urethrocele. When the urethra loses its normal support, it protrudes into the vagina. As a rule, there is a combination of urethro- and cystocele. Stress urinary incontinence
Almost 40% of women over 60 years old have this pathology. Some forms can be corrected surgically, but are often combined with loss of the posterior uterovesical angle. Before surgery, patients should be examined using a cystometrogram. Benign tumors
OVARIAN TUMORS
Follicular cysts
These are unruptured enlarged Graafian follicles; their rupture, twisting or spontaneous regression is possible. Corpus luteum cyst
Can be of considerable size (10-11 cm). Rupture of the cyst leads to severe blood loss, and sometimes vascular collapse occurs. Complaints and examination data are similar to the clinical picture of ectopic pregnancy. Endometrioma
Cystic forms of ovarian endometriosis. Wolffian duct rudiment
Small single-chamber cysts that do not originate from the ovaries; enlargement and twisting are rarely noted. Non-functioning tumors
Cystoadenomas
Serous cystadenomas - These are cysts with translucent walls containing clear fluid and simple ciliated epithelium. Adequate treatment represented by salpingo-oophorectomy or oophorectomy only. Mucous cystadenoma is a cystic tumor with viscous jelly-like contents. Malignancy of mucinous tumors is less likely than serous cystadenomas. About 20% of serous and 5% of mucous tumors have bilateral localization. Some cystomas are classified as borderline tumors, or adenocarcinomas with low malignant potential. The prognosis is usually favorable. For a unilateral process in women of reproductive age, unilateral adnexectomy is used. In a state known as abdominal pseudomyxoma, the abdominal cavity is filled with viscous mucus. The tumor grows from the mucous cystadenoma of the ovary or mucocele of the appendix. Histologically, benign local spread and infiltration of surrounding organs is determined. Treatment consists of bilateral removal of the ovaries and appendix. Teratoma
It occurs at any age, but is more common in patients between 20 and 40 years of age. Usually these are benign dermoid cysts, sometimes they have a dense consistency and then become malignant. In young women, ovarian cystectomy is preferable, if possible preserving the functioning tissue of the affected ovary. Cysts contain ecto-, meso- and endodermal tissues along with fat, which, if disseminated, can cause chemical peritonitis. A biopsy of the other ovary is performed when pathology appears. In approximately 12% of cases the tumor is bilateral. Brenner's tumor
These are rare fibroepithelial tumors. Epithelial elements are similar to Walthard's rudiments and appear in old age and have little potential for malignancy. Treatment: standard oophorectomy Meige syndrome
Ascites with hydrothorax, considered in connection with benign ovarian tumors with fibrous elements (usually fibroma), constitute Meige's syndrome. The causes are unknown, but ascites fluid arises from the tumor due to impaired lymphatic drainage from the ovary. Syndrome being treated removal of fibroids. Functioning tumors
Granulosa thecal cell tumor
Theca cell tumors (thecomas) are benign, but in the presence of granulosa cell elements they can become malignant. Granulosa cell tumors sometimes produce estrogen. Tumors occur at any age (from childhood to postmenopause), but more often in the elderly. Premature puberty or endometrial changes with a hormonally active tumor are combined. If the disease is detected in a woman of reproductive age and is limited to one ovary, then oophorectomy is sufficient. In elderly patients, the uterus and both ovaries are removed. Sertoli-Leydig cell tumors (archenoblastoma)
A rare but potentially malignant tumor with androgen production and masculinization. Usually occurs in women of reproductive age. In young patients with lesions of one ovary, unilateral oophorectomy is indicated. For elderly people with a bilateral process, hysterectomy and bilateral salpingo-oophorectomy are necessary. Struma ovary
Occurs in the ovary in the presence of thyroid tissue as the predominant element; hyperthyroidism is possible. Leiomyoma
The most common benign tumor in women, it never appears until menarche, grows during the reproductive period and regresses at menopause. Presents with pain, dysfunctional uterine bleeding, infertility, ureteral obstruction, bladder displacement and pressure symptoms. Leiomyoma can undergo degenerative changes, including calcification, necrosis, fatty degeneration and rarely sarcoma: Malignancy occurs in less than 1% of cases. For symptoms of invasive growth, myomectomy, total abdominal hysterectomy, or transvaginal hysterectomy is indicated. Adenomyosis
Adenomyosis is the growth of endometrial tissue in the myometrium, sometimes regarded as endometriosis of the uterine body. Thickening of the myometrium occurs, followed by enlargement of the uterus. Examination reveals dysmenorrhea with increasing uterine bleeding. Polyps
Polyps are local hyperplastic growths of the endometrium, which usually cause bleeding after menstruation or menopause. Treatment consists of removing polyps. Cervical lesions
Cervical polyps are often quite small and located on the outside. They are removed on an outpatient basis. Naboth cysts are cervical cysts with mucous contents. Usually harmless, asymptomatic and do not require surgical treatment. Pathology of the vulva
The term " leukoplakia" often used to refer to any white patches on the vulva. Lichen sclerosis and atrophy cause itching, which is not associated with premalignancy. Topical testosterone or steroid therapy reduces itching. Hypertrophic dystrophy can be benign (epithelial hyperplasia) or atypical, in which case dysplastic changes are detected. Carcinoma in situ of the vulva is clinically and histologically similar to carcinoma in situ of the cervix. The changes are limited to the squamous (squamous) epithelium of the vulva and are sometimes interpreted as Bowen's disease. Paget's disease of the vulva, developing from apocrine glandular elements, is combined with itchy red rashes. Histologically, large foam Paget cells are visible, similar to breast cells. Both Bowen's disease and Paget's disease are integral part vulvar carcinoma in situ, and treatment consists of wide excision of local tissue. Malignant tumors
OVARIAN TUMORS
Ovarian carcinoma
Ovarian cancer is histologically divided into epithelial, germ cell and stromal. Every year, 21,000 cases of epithelial cancer are diagnosed in the United States. Average age The patients are 61 years old; the 5-year survival rate for this diagnosis is 37%. Approximately 5% of patients with epithelial tumors come from families in which one or more first-generation relatives also had this pathology. In such families, prophylactic oophorectomy may be considered after the end of the childbearing period. However, primary peritoneal carcinomatosis also occurs in women after surgical intervention for prophylactic purposes. The International Federation of Gynecologists and Obstetricians gives a classification of ovarian cancer presented in table. 39.2. Most women at the time of diagnosis have stage III of the development of the tumor process. Treatment. Therapy for ecithelial forms of ovarian cancer consists of surgical resection based on the stage of the disease, followed by chemotherapy. Women with low-grade tumors in early stages (IA and IB) can only be treated with surgery. In a limited group of patients with unilateral lesions and histological confirmation of grade 1 or 2 differentiation, fertility can be preserved by adnexectomy and biopsy staging without removal of the uterus or contralateral ovary. In all other patients (stage IA, grade 3 and stage IB and higher), first surgical treatment (bilateral salpingo-oophorectomy, abdominal hysterectomy, staging and tumor resection). Table 39.2. Stages of ovarian cancer. International Federation of Gynecologists and Obstetricians (1986)
|
|
Characteristic
|
|
|
Growth limited by ovaries
|
|
|
Growth limited to one ovary, no ascites, no tumor on the outer surface, intact capsule
|
|
|
Growth limited to two ovaries, no ascites, no tumor on the outer surface, intact capsule
|
| IC |
The tumor is the same as in stages IA or IB, but is located on the surface of one or both ovaries, or a rupture of the capsule, or a tumor with ascites fluid containing malignant cells, or with positive peritoneal washings |
| II |
A growing tumor affects one or both ovaries and spreads throughout the pelvis |
| PA |
Spreads or metastasizes to the uterus or fallopian tubes |
| IIВ |
Spreads to other pelvic organs |
| IIС |
The tumor is the same as stage IIA or IIB, on the surface of one or both ovaries, or with rupture of the capsule(s), or with ascites fluid containing malignant cells, or with positive peritoneal washings |
| III |
The tumor affects one or both ovaries with peritoneum outside the pelvis, retroperitoneal or inguinal lymph nodes; superficial liver metastases equal to stage III; the tumor is limited to the pelvis, but with histologically verified spread to the lesser omentum or small intestine |
| IIIA |
The tumor is clearly limited to the pelvis without involvement of the lymph nodes, but with histological confirmation of involvement of the abdominal peritoneum |
| IIIB |
Tumor of one or both ovaries, histologically confirmed involvement of the abdominal surface of the peritoneum, does not exceed 2 cm in diameter, lymph nodes are intact |
| IIIC |
Peritoneal lesions greater than 2 cm in diameter or retroperitoneal or inguinal lymph nodes involved |
| IV |
The process involves one or both ovaries with distant metastases; if there is pleural effusion, there should be positive results tests showing stage IV; metastases to the liver parenchyma also indicate stage IV |
Staging. The stage of the process determines the extent of resection during surgery or biopsy of all tissues for possible tumor growth. Epithelial ovarian cancer spreads along the peritoneum through the lymphatic vessels. Most often, metastases are located in the omentum, para-aortic and pelvic (Lymph nodes. In case of ascites, it is necessary to take fluid for cytological examination. If there is no ascites, peritoneal lavages are performed while maintaining the water-electrolyte balance (injection of saline solutions or Ringer's solution) and lavage of the pelvic cavity , intestinal loops and subdiaphragmatic space. Patients with histologically confirmed grade 1 or 2 tumors of one or both ovaries (stage IA or IB) do not require postoperative treatment. The 5-year survival rate in this group of patients exceeds 90%. For grades 1-3 histologically, stage 1C clinically (peritoneal malignancy, tumor rupture, superficial discharge or ascites) or stage II, complete surgical removal tumors followed by a course of chemotherapy, irradiation of the entire abdominal wall or intraperitoneal administration of radioactive phosphorus (32 R). The 5-year survival rate approaches 75%. Women with stages III and IV of the process require a course of chemotherapy with cisplatin or carboplatin in combination with alkylating drugs or alkaloids such as Taxol. The 5-year survival rate can exceed 20%, and the 10-year survival rate can exceed 10%. Patients with little or no residual disease after primary surgery have a longer life expectancy on average than patients with non-removable tumor areas. Terms "reduction of tumor mass(decrease in tissue volume) or shield reduction" involve deliberate surgical removal of ovarian cancer, even if the operation is obviously non-radical. When the source of the disease after such resection of the tumor remains in the lymph nodes or plaques measuring less than 1-2 cm in diameter, this is called optimal treatment effect, with larger sizes - suboptimal.
Resection for advanced ovarian cancer. Successful resection of a tumor node 2 cm or less is possible in at least 50% of women with disease progression. Subsequent chemotherapy provides survival that is inversely proportional to the size of the unresected site and the time of the primary operation. Planned reoperations. Repeated laparotomy. It is quite difficult to determine the recurrence of ovarian cancer during or after treatment. Although CT and MRI examinations detect both small and nodules 2-3 cm in diameter, no technique can detect small nodules. Repeated operations are used as planned for examination purposes. They are valuable in determining the need to continue therapy, timing of reoperation, and prognosis. Other reoperations. Surgical resection of the tumor after chemotherapy or recurrence is called secondary cytoreduction.
The significance of secondary cytoreduction has not been established. If the patient fully responds to basic platinum combination treatment and the recovery period exceeds two years, reintroducing platinum chemotherapy is very effective. In such patients, surgical removal of the recurrent tumor will be beneficial. Palliative surgical treatment.
In most cases of advanced ovarian cancer, the cause of death is bowel dysfunction or obstruction. When intestinal obstruction occurs after a course of chemotherapy, the prognosis is poor. In patients with such manifestations, survival after surgical treatment is significantly reduced. Often, when treating such pathology, percutaneous or endoscopic positional gastrotomy is considered the best approach, intravenous administration liquids or parenteral. Laparoscopy for ovarian cancer. Our ability to successfully resect large ovarian tumors using laparoscopic techniques is limited. However, the role of laparoscopy in staging and treatment of ovarian malignancy is expanding. For oophorectomy and removal of pelvic and para-aortic lymph nodes, endoscopic techniques are used. Tumors with low malignancy potential
These are epithelial tumors with an average possibility of malignancy - between benign pathology and obvious malignancy. Most of them serous type, microscopically differ from invasive cancer by insufficient stromal growth. The average age at diagnosis of this pathology is approximately 10 years younger than that of patients with epithelial cancer. As a rule, stage I is diagnosed. Surgical treatment includes abdominal hysterectomy and bilateral salpingo-oophorectomy if childbearing is not possible; if persists, then unilateral salpingo-oophorectomy. About 85% of patients with stage III or IV disease have a 5-year survival rate after complete surgical resection. There is little evidence that radiation and chemotherapy given after surgery improve survival. Germ cell tumors
Tumors occur in women in the first 30 years of life and grow rapidly, manifesting as a distension symptom and a neoplasm in the abdominal cavity. The process is usually unilateral and tends to spread to the para-aortic lymph nodes. Dysgerminoma is similar to testicular seminoma and consists of undifferentiated germ cells. Bilateral damage is observed in 10% of patients; the disease is rarely combined with an increase in the level of human chorionic gonadotropin or lactate dehydrohexase activity. This is the most common malignant tumor diagnosed during pregnancy Other germ cell tumors: immature teratoma, endodermal sinus or yolk sac tumor, mixed tumors, embryonal carcinoma or choriocarcinoma. The first can be combined with an increase in the level of a-fetoprotein. Its increased concentration is detected in patients with endodermal sinus tumors and mixed tumors containing this component. Embryonic carcinoma Increases the level of both a-fetoprotein and human chorionic gonadotropin; choriocarcinoma secretes the latter. In addition to complete resection of stage 1-1 underdeveloped teratoma and stage I dysgerminoma, All patients require a course of chemotherapy. Three courses of treatment with platinum and an etoposide-containing combination are sufficient for patients with a completely resected tumor. The recovery rate in this group of patients is close to 90%. Cervical cancer
Every year in the United States, about 16,000 cases of cervical cancer are registered, and 5,000 patients die. Risk factors: multiple sexual partners, early age first sexual intercourse, early first pregnancy. It is believed that the human papillomavirus identified in cervical dysplasia and carcinoma in situ, as well as all previous factors, can cause invasive cancer with metastasis to the lymph nodes. A screening program can reduce the incidence of invasive cancer in countries where cervical cytology testing is widely used. The use of this method increases the frequency of detected premalignant intraepithelial diseases, dysplasia and carcinoma in situ. 80% of all cervical cancers are squamous cell (squamous cell, squamous cell) and grow at the border of squamous and columnar epithelium. The remaining malignant tumors of the cervix grow from the endocervical canal and are classified as adenosquamous, or adenosquamous, carcinomas. Other rare histological variants that have a poor prognosis are neuroendocrine small cell carcinoma and pure cell carcinoma. The latter is often combined with maternal intake of diethylstilbestrol. Staging. The International Federation of Gynecologists and Obstetricians determines the stages of cervical cancer based on clinical examination, intravenous pyelography and chest radiography, which is presented in Table. 39.3. In addition to patients with stage IVA and distant metastatic tumors, in the United States all patients with stage IV continue to receive primary cervical therapy. Treatment.Intraepithelial or preinvasive diseases. If pathological changes are found during cytological examination of the cervix, patients should undergo colposcopy and biopsy. Cervical intraepithelial neoplasia is treated in several ways. Significant epithelial damage and a higher level of dysplasia result in a high failure rate. The most favorable treatment method is vaginal or abdominal hysterectomy. Surgery is usually reserved for patients with an advanced process or epithelial damage high degree. It is performed when the disease relapses after conservative therapy in patients who have other indications for hysterectomy. In most cases of this pathology, a cervical biopsy is indicated. Table 39.3. International classification of cervical cancer
|
Stage
|
Clinical manifestations
|
|
|
Carcinoma in situ
|
|
|
Carcinoma is clearly limited to the cervix (spread into the body can be neglected)
|
|
|
Preclinical cervical carcinoma is diagnosed. only based on microscopy results
|
|
|
Minimal microscopically clear penetration into the stroma
|
|
|
Damage is determined microscopically and can be measured. The upper limit of penetration depth may not exceed 5 mm from the main epithelium, also superficial or glandular, from which the tumor grows; the second value - horizontally - does not exceed 7 mm. Larger damage should be assessed as IB
|
|
|
Defeats large sizes than in stage IA2, are either clinically visible or not. Existing spatial involvements do not extend beyond the stage, but can be noted to determine the subsequent therapeutic effect
|
|
|
The vagina is affected (not in the lower third) or there is infiltration of the parametrium, but not along the lateral surfaces
|
|
PA
|
The vagina is affected, but there is no evidence of changes in the parametrium
|
|
IV
|
Infiltration of the parametrium is detected, but not on the outer surface
|
|
|
The lower third of the vagina is affected or the process spreads from the pelvis
|
|
IIIA
|
The lower third of the vagina is affected, but not the outer surface of the pelvis if the parametrium is involved
|
|
IIIB
|
Damage to the parametrium on one or both sides
|
|
Shs
|
Obstruction of one or both ureters, detected by intravenous pyelography, in the absence of other criteria characteristic of stage III
|
|
|
Spread from the external genitalia
|
|
|
Damage to the mucous membrane of the bladder or rectum
|
|
|
Distant metastases or pathology confirmed outside and outside the pelvis
|
More conservative methods Treatments for cervical intraepithelial neoplasia include snare wire excision, laser ablation, and cryosurgery. Microinvasive cervical cancer. The International Federation of Gynecologists and Obstetricians divides microinvasive cancer into “early” invasive cancer (stage IA1) and a tumor that is less than 5 mm in thickness and has a lateral extension of 7 mm (stage IA2). The differences between stages IA2 and IB according to the International Classification are not adequate, since both require regional therapy from the moment of detection of metastases in the lymph nodes. Many doctors prefer the original Society of Gynecologic Oncology system, in which a stage IA tumor (microinvasive cancer) can spread more than 3 mm and have incomplete invasion of the capillary or lymphatic space. Stage IB includes all other clinically confirmed cervical cancers. The advantage of this classification is that there is a clear separation of stage I in the two treatment groups. Simple or superficial hysterectomy without lymphadenectomy is sufficient treatment for stage IA. The 5-year survival rate in these patients is close to 100%. In selected cases, cervical cone biopsy or electrosurgical excision may help. Early invasive cervical cancer (stages IB and ON THE). Tumors of these stages have a risk of developing metastases to the pelvic (10-15%) and periarrheal (5%) lymph nodes. An effective method of treatment in at0t, reri-fi is radical hysterectomy with pelvic lymphadenectomy and subsequent radiation therapy. Predominantly local cervical carcinoma (stages IIB-IVA). These types of carcinomas are primarily treated with radiation therapy" with Treatment consists of a combination of external therapy of the small pelvis (teletherapy) from a powerful energy source and a local dose delivered to the cervix and parametrium; applications with cesium are used. The recovery rate in the PV and IIIB groups is 65 and 35%, respectively. Recurrence of ovarian cancer. Local recurrences after previous surgery are being treated more effectively external and internal radiation therapy. Recurrence of distant metastases may get treatment palliatively with local radiation or chemotherapy. ENDOMETRIAL CANCER
The most common malignant pathology of the female genital organs. In the United States, 33,000 new cases are diagnosed annually, and 4,500 patients die. Risk factors: obesity, sugar diabetes, hypertension, low number of births in history, early menarche, late menopause. Excess estrogen is important for the development of endometrial cancer and its precancerous diseases, such as endometrial hyperplasia. Women who have excess estrogen during menopause have a 6-fold increased risk of endometrial cancer if they do not use progesterone-type drugs. Endometrial hyperplasia is divided into single And complex, with atypia or without her. Atypical complex hyperplasia most likely gives rise to frank adenocarcinoma. The preferred treatment method is hysterectomy. Women with somatic diseases (in this case, surgical treatment is not possible) are treated with progesterone-type drugs, such as megestrol or medroxyprogesterone acetate. Both endometrial hyperplasia and carcinoma are often accompanied by uterine bleeding during postmenopause or menopause. Treatment. Endometrial cancer by stages, according to the classification of the International Federation of Gynecologists and Obstetricians, is presented in table. 39.4. Stage I of the disease is successfully treated with abdominal hysterectomy and bilateral salpingo-oophorectomy. Radiation therapy may be required, which when used before surgery reduces the risk of recurrence. Metastases to the pelvic lymph nodes occur in patients in 12% of cases and are limited to the uterus. Risk factors for tumor spread to lymph nodes include significant histological grade of involvement (G2, 03); low level progesterone receptors, deep endocervical invasion, adnexal extension, endocervical extension, and uncommon histological variants such as papillary serous or clear cell carcinoma. In the latter cases with a high probability of spread to the pelvic lymph nodes (histological level 3 lesion, involvement of "/3 layers of the myometrium or uterine serosa, high risk of histological subtypes), the common iliac and para-aortic lymph nodes, especially those lying lateral to the radiation field, should be examined. An important element in determining the stage of the process is a cytological examination of the abdominal fluid. In approximately 12% of patients, malignant cells are found during examination, which increases the risk of developing intra-abdominal insufficiency (pathology of the abdominal organs). In patients with PV and stage III of the disease, the question o radiation therapy pelvis in the preoperative period (if surgical treatment is impossible or difficult). Radiation becomes the method of choice when there is a high risk of surgery, but the results are worse than after surgery. Progressive endometrial cancer or its relapse is sensitive to therapy with progesterone drugs or tamoxifen in 30% of the control group of patients. VULVA CANCER
Among all cancers of the female genital area, vulvar cancer accounts for 5%. Risk factors: elderly age, smoking, previous intraepithelial or invasive (squamous or squamous cell) cancer of the cervix or vagina, chronic vulvar dystrophy, immune deficiency. In preinvasive and invasive squamous carcinomas of the vulva, a DNA virus resembling human papillomavirus has been detected and identified. Vulvar squamous carcinoma spreads through the lymphatic system. In 1988, the International Federation of Gynecologists and Obstetricians identified the stages of vulvar cancer, presented in table. 39.5. Table 39.4. Stages of uterine cancer. International Federation of Gynecologists and Obstetricians (1988)
|
Stage
|
IVA G123
|
The tumor invades the bladder and/or intestinal mucosa
|
|
|
Distant metastases, including intra-abdominal and/or inguinal lymph nodes
|
HISTOLOGICAL LEVELS OF DIFFERENCE
Cases are grouped by degrees adenocarcinoma differentiation
|
| G1 |
5% or less non-squamous or non-mular solid growth structure
|
| G2 |
6-50% non-squamous or non-mular solid growth structure
|
| G3 |
More than 50% non-squamous or non-mular solid growth structure
|
| CHARACTERISTIC FEATURES OF PATHOMORPHOLOGICAL GRADES
Significant atypia of cell nuclei, unsuitable in structure, increases the degree of damage.
For serous and pure cell adenocarcinomas and squamous cell carcinomas, the previous nuclear grade is taken.
Adenocarcinoma with squamous features is graded according to the nuclear grade of the glandular component.
|
| RULES FOR DETERMINING STAGE
Since there is currently a surgical classification of uterine cancer, the previous method of determining stages is not used (periodic curettage was required to determine the difference between stages I and II).
It is appreciated that a small number of patients with endometrial cancer will be treated with radiation first. In this case, the clinical stages were adapted by the International Federation of Gynecologists and Obstetricians in 1971 and are still used, but the significance of this system is of historical interest. Ideally, the width of the myometrium should be comparable to the width of tumor invasion.
|
|
Stage
II T 2 N 0 M 0
|
The tumor is limited to the vulva and/or perineum, more than 2 cm in size. No metastases to lymph nodes
|
Stage III
T 3 N 0 M 0
T 3 N 1 M 0 |
Tumor of any size:
1) extends to the lower parts of the urethra and/or vagina, or anus, and/or...
|
T 1 N 1 M 0
T 2 N 1 M 0 |
2) unilateral metastases to the lymph nodes.
|
Stage IVA
T 1 N 2 M 0
T 2 N 2 M 0 T 3 N 2 M 0
T 4 any N M 0
|
The tumor invades any organs: the upper parts of the urethra, the mucous membrane of the bladder and rectum, the pelvic bones and/or bilateral damage to the lymph nodes
|
Stage IVB
Any T
Any N
Any Mj |
Distant metastases, including pelvic lymph nodes
|
Treatment. For most vulvar carcinomas, the preferred treatment is radical vulvectomy and inguinal lymphadenectomy through separate incisions. Squamous or squamous vulvar cancer less than 2 cm in diameter, no more than 1 mm in thickness and histological grade 1 or 2 is associated with a very small risk of developing metastases to the inguinal lymph nodes; deep and wide excision is sufficient for adequate treatment. In such cases, inguinal lymphadenectomy may not be performed. In recent years, locally progressive pathology of the vulva has also been successfully being treated external focused irradiation combined with radiosensitive drugs such as cisplatin and 5-fluorouracil. In conclusion combination therapy the affected surface is widely excised. Rare vulvar tumors
Medanoma. Lesions less than 1 mm thick or Clark II can be treated conservatively with wide local excision. The effectiveness of inguinofemoral lymphadenectomy remains controversial. Intraepithelial diseases. These include Bowen's disease, papulosis, vulvar intraepithelial neoplasia, and carcinoma in situ, which can be successfully treated by wide excision of the affected epithelium. In cases of diffuse intraepithelial disease, a so-called cutaneous vulvectomy and skin thickness dissection may be required. Carbon dioxide laser and electrosurgical loop are effective. Paget's disease is an uncommon epithelial or invasive process characterized by the presence of distinct Paget's cells in the affected epithelium. Treatment This type of lesion consists of wide excision. In rare cases, Paget's disease is combined with underlying invasive adenocarcinoma, in which case radical vulvectomy and revision of the groin area are indicated. Bartholin's gland carcinoma accounts for less than 1% of all cases of vulvar malignancy and is treated in the same way as squamous adenocarcinoma. Gynecological surgeries
Scraping
Cervical dilatation and uterine curettage was one of the most common surgical procedures performed in the United States because it provided a diagnosis for dysfunctional bleeding. Manipulation is necessary to stop profuse uterine bleeding. Indicated for the removal of endometrial polyps or treatment at the end of pregnancy, as well as for the removal of placental tissue after abortion or childbirth. The main complication of curettage is uterine perforation, which is diagnosed by the absence of resistance during stretching or by curettage at the point where perforation can be expected. Tactics treatment is of a wait-and-see nature. In recent years, aspiration curettage has become popular for incomplete abortion, chorionic adenoma and therapeutic abortion. Endoscopic surgery
For many years, endoscopic techniques have been used to perform tubal sterilization and tubal restoration. Currently, the technique is used in the treatment of endometriosis, ectopic pregnancy, uterine fibroids, and pelvic pain. Laparoscopy is absolutely contraindicated in cases of intestinal obstruction, severe ileus, very large tumors abdominal cavity, diaphragmatic hernia and severe cardiopulmonary diseases. Relative contraindications: massive obesity, severe intestinal diseases and multiple previous abdominal surgeries in history.
|
The importance of medical history for diagnosing gynecological diseases is extremely high. The female genital area is very closely connected with other organs and systems; its pathology can never be separated from the whole organism. I. P. Pavlov and his student A. G. Ivanov-Smolensky attached extremely great importance to the anamnesis. When starting to collect anamnesis of a gynecological patient, it is necessary to learn how to assess various complaints and symptoms. To collect anamnesis from the greatest completeness and expediency, it is best to use a specific scheme, which is included in clinical history diseases. The gynecological clinic of the State Pediatric Medical Institute used a special medical history form, which contains an anamnesis diagram that is filled out when receiving inpatient and outpatient patients ( the gynecological examination form will be discussed in detail in the next article).
Let us dwell in a little more detail on individual issues of the anamnesis and medical history of the gynecological patient as a whole. From passport information, special attention should be paid to the patient’s age, since this is important for the age-related pathology of a woman, as well as for carrying out rational therapy, which may be different at different ages. Occupation is of great importance, since some types of gynecological diseases are associated with a specific profession.
From the medical history, the doctor’s main questions are the following two: 1) what the patient is complaining about (it is necessary to accurately determine the nature and essence of the complaints); 2) when the disease began, how long he considers himself sick. Further details about this disease are clarified after a life history, family history and a survey about the woman’s basic functions.
From the life history it is found out living conditions, in which the woman is, diseases suffered in childhood, general, gynecological, postpartum and venereal diseases; in addition, it is necessary to find out whether the husband had any serious and socially dangerous diseases (alcoholism, tuberculosis, syphilis).
Then they move on to the history of the so-called “basic functions” of the woman, of which there are four.
1. First, they dwell on the history of menstrual function, and be sure to find out the time of the onset of the first menstruation. Next they ask whether menstruation began immediately, how it proceeded - cyclically or intermittently; how many weeks came and how many days lasted; passed with pain or painlessly. Late onset of menstruation and long breaks between them indicate general underdevelopment of the woman’s body or underdevelopment of the genital organs. You should also find out whether your periods have changed after marriage (which happens, for example, when infected with gonorrhea). Finally, the date of the last menstruation is determined from the anamnesis. In the elderly, the time of onset of menopause or menopause and the characteristics of the course of the latter are determined.
2. When interviewing a woman about her labor function, you should find out the total number of pregnancies, how many of them ended in childbirth and abortion; were there any premature births, artificial or spontaneous abortions; when was your last pregnancy (birth or abortion); were there any complications of pregnancy, childbirth or abortion, what kind; number of children. A large number of pregnancies, especially those ending in abortions, is typical for patients with cervical cancer, while a small number or infertility are typical for patients with uterine fibroids. Multiple induced abortions can cause infertility and inflammatory diseases of the genital organs.
3. The nature of the discharge - excretory function - from the urethra, cervical canal, vestibular glands, vagina and uterus is considered pathological in cases where normal discharge is produced in large quantities (hypersecretion) or has a foul odor, or if pus, blood are mixed with the leucorrhoea, serous fluid. - From the anamnesis, it becomes clear how long this suffering has been, whether the discharge stains the underwear, what kind of treatment was carried out for the leucorrhoea.
4. Anamnesis of sexual function is especially important in patients with neuroses, frigidity, uterine fibroids, inflammatory processes genitals. It turns out whether there is sexual desire (libido), orgasm and sexual satisfaction. It is also important to find out whether there is pain and contact bleeding during sexual intercourse, as well as a method of preventing pregnancy, paying attention to coitus interruptus, if used.
After receiving the specified information, we can assume that the anamnesis has been largely collected. Next, it is necessary to collect additional anamnesis regarding the functions of the bladder and intestines (especially the rectum); their improper function affects the position of the genital organs and their function. An anamnesis of the four functions of the female body facilitates further, more detailed questioning about this disease. The patient must provide detailed information about her disease, its clinical course, therapy performed, etc., which may be important for the correct diagnosis and further treatment.
Main symptoms of gynecological diseases. Examination methods in gynecology.
I. Main symptoms of gynecological diseases.
For the recognition of gynecological diseases, data on menstrual, reproductive, secretory, and sexual functions are of great importance.
Menstruation disorders often occur when the function of the nerve centers that regulate the activity of the endocrine glands, which are involved in preparing for pregnancy and carrying it to term, is impaired. The functional instability of this system can be congenital or acquired as a result of damaging factors (diseases, stressful situations, poor nutrition) in childhood and during puberty.
Gynecological diseases can be both the cause of reproductive dysfunction (infertility, spontaneous abortions, abnormalities of labor) and their consequence (inflammatory diseases that occur after abortion and childbirth, neuroendocrine disorders after heavy bleeding in women in labor and postpartum, consequences of obstetric injuries).
Pathological secretion (leucorrhoea) can be a manifestation of disease in different parts of the genital organs.
Leucorrhoea is distinguished:
Tubal (emptying hydrosalpinx)
Uterine (or corporal) (endometritis, polyps, initial stage endometrial cancer)
Cervical leucorrhoea (endocervicitis, eroded ectropion, erosion, polyps)
Vaginal.
In healthy women, there is no visible discharge from the genital tract. The processes of formation and resorption of vaginal contents of the vaginal mucosa are completely balanced. Vaginal leucorrhoea appears when pathogenic microorganisms are introduced (poor sexual hygiene, gaping of the genital slit after perineal tears, etc.), unreasonable vaginal douching, and the use of irrational contraceptives.
Data on sexual function deserve great attention. Sexual function disorders are observed in many gynecological diseases. Sexual desire, sexual feeling and satisfaction characterize the maturity of women's sexual function. The absence of these indicators of sexual function is observed with gonadal dysgenesis and other endocrine disorders, as well as for many gynecological diseases.
Pain during sexual intercourse is typical for:
endometriosis (retrocervical)
inflammatory diseases
colpitis
salpingo-oophoritis
hypoplasia of the genital organs
vaginismus
It is necessary to know about dysfunctions of adjacent organs: the condition of the urinary tract and intestines (the presence of urethritis, cystitis, intestinal hypotension, flatulence and others). These disorders also occur in many gynecological diseases.
II.Methods of gynecological examination.
Age at which menstruation began (menarche)
Regularity of the menstrual cycle
Duration of menstruation
Duration of the menstrual cycle from the first day of the last menstruation to the first day of the next menstruation
Example:
Menstruation began at the age of 13, lasts 5 days, the duration of the menstrual cycle is 28 days.
Number of births, with age and weight of children at birth
Any pathology during pregnancy, childbirth or the postpartum period
Number of miscarriages, indicating gestational age, date of miscarriage, presence of complications
Any termination of pregnancy, indicating the duration and method of termination.
sexual intercourse;
any discomfort or pain in cases of infertility;
whether sexual intercourse is normal;
frequency and timing of sexual intercourse during the menstrual cycle.
using an intrauterine device
the use of oral contraceptives is particularly important because of their possible effect on menstruation.
abnormal menstrual bleeding is observed;
cyclical bleeding;
the amount of blood lost (more or less than usual);
number of sanitary towels or tampons used;
discharge of blood clots or non-coagulating blood;
presence of pain during blood loss;
pelvic pain: location, nature and relationship with menstruation.
the relationship with the husband or sexual partner is clarified;
family problems are identified;
psycho-emotional overload at home and at work.
You can get a lot of information about the general condition of the patient by observing her while taking anamnesis. The patient should be monitored on a case-by-case basis. For example, it is necessary to note what a woman looks like: sick or healthy, high or low nutrition. It should be noted whether the patient answers questions readily or reluctantly, trying to hide something or talking about symptoms that she thinks might lead to a diagnosis she fears. Is she depressed, anxious, or suffering from some kind of emotional disorder, the symptoms of which are an unconscious expression of the need for help.
Examination of the abdominal wall.
The patient should lie flat, and if the abdomen is swollen and there is tension in the muscles of the anterior abdominal wall, then the patient should bend her knees in order to reduce muscle tension. The bladder should be empty.
Inspection.
The size and shape of the abdomen is noted. Enlargement of the abdomen in the midline may indicate the presence of a tumor of the uterus or ovaries. An increase in the size of the abdomen along the periphery is possible with ascites. Attention is paid to the condition of the skin, the presence of the white line of the abdomen, rashes, pigmentation or scars.
Palpation.
The abdomen should always be examined with a warm hand and preferably with the flat of the palm rather than with the fingertips, since then deep palpation can be performed painlessly for the patient.
Tumors arising from the pelvis, unless they are impacted or fixed by adhesions, can easily move from side to side (but not up and down), and in this case it is impossible to palpate the lower edge of the tumor. Tumors can be solid or cystic (that is, solid or liquid). If liquid tumors are large enough, then they are easily palpated with a flat palm and can be easily felt. Ascites produces a fluid tremor, which is determined by the presence of dullness to percussion.
Percussion
Percussion allows you to decide whether the swelling is in contact with the abdominal wall and is causing the dull sound, or whether it is loops of intestine located between the tumor and the abdominal wall. If, during percussion of the abdomen, a ringing sound is detected in the center and a dull sound on the sides, and this dull sound moves when the patient’s position changes, then the presence of free fluid can be diagnosed.
Auscultation
When listening with a stethoscope, intestinal peristalsis is usually heard. A "silent" abdomen indicates intestinal paralysis and is found in cases of shock, generalized peritonitis and postoperative paralytic ileus.
Examination of the external and internal genitalia gives a lot of information about the patient. The presence of hypoplasia of the labia minora and majora, pallor and dryness of the vaginal mucosa are clinical manifestations of hypoestrogenism. “Juicy” mucous membrane, cyanotic color of the vulvar mucosa, abundant transparent secretion are signs of increased estrogen levels.
Inspection in mirrors.
Visual inspection of the vagina is performed using mirrors. The examination should be carried out carefully without causing pain to the patient. This requires a small amount of sterile lubricant. It should be taken straight from the tube so that it does not become contaminated and cause cross-infection. The lubricant must be transparent, so that secretions can be differentiated on it, and should not contain antiseptics that interfere with bacteriological examination.
Two types of mirrors are used: the Cusco double-leaf mirror and the Sims spoon-shaped mirror.
Sims Mirror
designed to detect pysovaginal fistulas. It consists of two concave blades of different sizes, connected by a handle.
Double-leaf mirror of Cusco
consists of two blades fixed together. This makes it possible to perfectly examine the cervix and vaginal mucosa. The doctor's hands remain free.
Vaginal examination.
A vaginal examination is the most confidential examination in medicine. It is very important to gain the patient's trust before the examination. The presence of an accompanying woman, a full explanation of how the examination will take place, a caring attitude towards the patient, empathy for her feelings and respect for her dignity - all this will help the patient relax and achieve mutual understanding. A vaginal examination consists of the following: palpation of the vagina, vaginal part of the cervix, bimanual palpation of the pelvic organs.
A recto-vaginal examination is of great importance. This study is recommended for tumors of the female reproductive system.
Widely used in gynecology to determine the functional state of the reproductive system.
The calculation of the karyopyknotic index (KPI) is used - in phase I, during the period of ovulation, and in phase II of the menstrual cycle. CPI is the ratio of superficial cells with a bright pyknotic nucleus to the total number of superficial cells that are formed under the influence of estrogens.
A smear is taken on the hormonal speculum from the anterior-lateral vaginal vault. Basal, intermediate, and superficial cells are identified.
Basal cells are determined during menopause, during treatment with androgens.
In phase I of the menstrual cycle and towards ovulation, growth of surface cells is observed. (0/30/70)
In phase II of the cycle (estrogens decline), intermediate cells 0/60/40 predominate.
Measurement basal temperature(physiological method of contraception Knaus - Ogino).
Symptom of mucus arborization (fern symptom).
In modern gynecological practice, radioimmunoassays (RIA) are used to determine blood plasma protein hormones: glutotropin, follitropin, prolactin and steroid hormones: estradiol, progesterone, testosterone, cortisol and others.
The content of hormones and their metabolites in urine is rarely determined in modern practice. In recent years, when examining women with manifestations of hyperandrogenism and conducting tests, instead of determining 17-ketosteroids in urine, the content in the blood plasma of dehydroepiandrosterone (DHEA) and its sulfate (DHEA-S) and 17-hydroxyprogesterone, precursors of testosterone and cortisol, respectively, and testosterone itself are examined. The determination of pregnanediol, a metabolite of progesterone, in urine was also inferior to the study of progesterone in the blood.
Instrumental diagnostic methods.
When examining patients, microscopic examination and cultural methods for diagnosing discharge of the urethra, cervical canal and posterior vaginal fornix are of great importance in order to identify genital infections.
To identify pathogens, immunochromatographic and enzyme immunoassay diagnostic methods are widely used.
For an endometrial biopsy, tissue can be obtained by using a small suction aspirator (vibratory aspirator) without general anesthesia.
Endoscopic diagnostic methods.
Colposcopy
Hysteroscopy
Laparoscopy
Colposcopy:
simple and advanced
Examination of the vaginal part of the cervix. This colposcopy is indicative in nature. The shape, size of the neck and external pharynx, color, relief of the mucous membrane, the border of the squamous epithelium covering the neck and the columnar epithelium of the cervical canal are determined.
The examination is carried out after treating the cervix with a 3% solution of acetic acid, which causes short-term swelling of the epithelium, swelling of the cells of the spinous layer, contraction of subepithelial vessels and a decrease in blood supply. The action of the acid continues for 4 minutes. After studying the colposcopic picture of the cervix, a Schiller test is performed - smearing the cervix with a cotton swab moistened with 3% Lugol's solution. Iodine, which is contained in the solution, colors glycogen in the cells of healthy, unchanged squamous epithelium of the cervix in a dark brown color. Thinning cells (atrophic age-related changes), as well as pathologically altered cells in various dysplasias of the cervical epithelium, are poor in glycogen and are not stained with iodine solution. Thus, areas of pathologically altered epithelium are identified and areas for targeted biopsy of the cervix are designated.
Colpomicroscopy.
Intravital histological examination of the vaginal part of the cervix. It is performed using a contrast luminescent colpomicroscope, the tube of which is brought directly to the cervix
Hysteroscopy.
This procedure is used to examine the uterine cavity. A small fiber optic telescope is passed through the cervical canal into the uterine cavity, which fills with fluid or gas. Hysteroscopy is used to identify endometrial polyps, intramural and submucous myomatous nodes, septa in the uterine cavity, identify internal endometriosis, and foreign bodies in the uterine cavity. This method is highly informative for diagnosing endometrial cancer. Biopsies or septal incisions can be made with this instrument. A hysteroscope can be used to access the interstitial end of the fallopian tube.
Laparoscopy.
Examination of the pelvic organs endoscopically was previously carried out through the posterior vaginal fornix (culdoscopy). In this case, the patient was in the knee-elbow position. This method has been replaced by the method of inserting an endoscope with a fiberoptic system and a small telescope through the anterior abdominal wall (laparoscopy). This ensures an excellent overview of the pelvic organs.
Indications for diagnostic laparoscopy.
Clarification of the patency of the fallopian tubes and identification of the level of occlusion (performed simultaneously with chromoperturbation).
Clarification of the diagnosis of polycystic ovaries.
Clarification of the nature of uterine development abnormalities.
Finding out the causes of pelvic pain.
Clarification of the causes of infertility.
Coagulation of endometriosis foci.
Wedge resection of polycystic ovaries.
Coagulation of polycystic ovaries.
Separation of adhesions in chronic salpingitis without disrupting the patency of the fallopian tubes.
Clamping, ligation or dissection of the fallopian tubes for contraceptive purposes.
Removal of small ovarian cysts, conservative myomectomy.
Hysterectomy
Plastic surgeries with laparoscopic assistance.
Emergency indications for laparoscopy
Differential diagnosis between acute adnexitis and appendicitis.
Suspicion of rupture or microperforation of the pyosalpinx.
Differential diagnosis between inflammation of the appendages and a progressive or interrupted ectopic pregnancy or ovarian apoplexy.
Ultrasound diagnostic methods.
On modern stage Ultrasound diagnostic methods are widely used in gynecological practice .
The examination can be carried out with a transabdominal probe (the bladder must be full) or transvaginally (the bladder must be empty). The uterus, ovaries, fallopian tubes, and ovarian tumors are well identified. This method is especially useful in differentiating solid from serous lesions. During the menstrual cycle, the growth of the Graafian follicle can be observed and the thickness of the endometrium can be measured. This way you can confirm the time of ovulation. Ultrasound examination is used to determine any early intrauterine or ectopic pregnancy, and to determine the location of the intrauterine contraceptive device.
You can also determine the extent of the spread of the malignant disease and the effectiveness of treatment. This method is now used to screen for ovarian cancer in healthy women.
X-ray examination methods.
Skull examination.
X-ray examination of the skull is widely used in the diagnosis of neuroendocrine diseases. To diagnose a pituitary tumor, an x-ray examination of the shape, size and contours of the sella turcica (bone bed of the pituitary gland) is performed. On a targeted photograph of the sella turcica or on a general craniogram, the sagittal, i.e., the largest anterior - posterior size of the sella (≈9-15 mm) is measured. The vertical size, or height of the sella, is measured by a line running from the deepest point of the bottom to the point of intersection with the diaphragm saddles The average vertical size is 9 mm. (from 7 to 12 mm.)
Panoramic photo of the pelvis.
A simple x-ray examination of the pelvis can sometimes help determine the location of the intrauterine device and identify calcification of tumors in the pelvic organs.
Cervico-hysterosalpingography, hysterosalpingography
– injection of a water-soluble contrast agent into the cervical canal, uterine cavity and fallopian tubes.
Intravenous pyelography –
used to diagnose displacement or obstruction of the ureters or bladder.
Computed tomography and magnetic resonance – can be used to study abdominal and pelvic tumors and to monitor (evaluate) the effectiveness of their treatment.