Conization is an operation to remove an area of altered tissue of the cervix and cervical canal. The removed fragment has a cone shape. The operation is performed to prevent the degeneration of altered tissues into a malignant form. Conization of the cervix can be performed for diagnostic purposes.
The operation is performed in cases of visible pathological changes in the cervix and in the presence of cervical epithelial dysplasia in smears.
Among the indications for the procedure, the main ones are:
- pathological changes in the cervix;
- laboratory confirmed dysplasia of 2-3 degrees;
- negative result of examination of discharge from the cervix.
- changes in the epithelium identified during colposcopic examination;
- dysplasia 2-3 degrees;
- eversion of the mucous membrane of the cervical canal (ectropion);
- erosion;
- presence of polyps;
- scar deformities;
- leukoplakia;
- recurrence of dysplasia after previous treatment with other methods.
Surgery may be performed to clarify the diagnosis. The extracted area is sent to the laboratory for histological analysis and, based on its results, the presence or absence of cervical cancer is judged.

Contraindications
The operation will not be performed if the woman has:
If there are contraindications, treatment is carried out, and conization of the cervix is postponed until the pathology is eliminated.
The purpose of conization
The main goal of surgical intervention is to remove pathologically changed tissues and prevent the process from degenerating into a malignant form.
The procedure allows for diagnosis and treatment of the disease.
- During the operation, the doctor removes the affected, affected area of the cervix within healthy tissue.
- The material is sent to the laboratory for histological examination.
- If, as a result of examination of healthy areas, cancer or dysplasia is not detected, then the pathology is considered completely cured.
- Conization will be considered diagnostic if the results raise doubts about the complete removal of pathological tissues with signs of dysplasia or invasive cancer. In this case, we will talk about others possible methods fight the disease.
Types of surgery

IN medical practice The most commonly used treatment methods are:
- electrocoagulation (loop electroconization);
- radio waves;
- laser;
- surgical knife.
The use of loop electrocoagulation may cause a small percentage of complications.
Radiosurgery
IN Lately Most doctors prefer treatment with radio waves. For the radio wave technique, the Surgitron apparatus is used. Tissue destruction is carried out under the influence of currents high frequency. Using a loop electrode of a suitable size, the affected area is cut out, capturing 3-4 mm of healthy tissue around the lesion and to a depth of up to 8 mm.
On to the pros radio wave therapy can be attributed:
- possibility of using local anesthesia;
- lack of bleeding due to coagulation of blood vessels;
- absence high temperature in the destruction zone allows you to minimize the risk of burns;
- the possibility of taking complete material for histological examination;
- the percentage of complications after the procedure is minimal.
Healing after conization of the cervix with radio waves lasts on average no more than a month. IN postoperative period There may be pain in the lower abdomen and scanty bloody issues. There is no need to be afraid of this - this is a normal phenomenon.
Using a laser
Laser surgery is less traumatic. This technique is expensive and high-tech.
The benefits of laser therapy include:
- the ability to accurately dose the depth of destruction;
- no risk of infection, since the laser beam has a sterilizing effect;
- Surgery is allowed for extensive lesions;
- There is no risk of bleeding, since coagulation of blood vessels occurs under the influence of the laser.
Among the disadvantages of the procedure:
- high risk of burns to healthy tissues;
- it is preferable to perform the operation under general anesthesia so that it is possible to completely immobilize the patient;
- high cost of the procedure.
Their presence is due to the fact that not every surgeon is able to perform such an operation. Rehabilitation after laser therapy proceeds without any special features and, as a rule, is quite successful.
Using a scalpel
This method is used less frequently than others due to increased risk complications (perforation, bleeding, scarring). However, it is the use of a knife that allows one to obtain better quality material for histological examination.
Loop electroconization
Excision of the affected tissue is carried out with a loop electrode. The procedure is low cost, so it is often used in gynecology. But, electroconization has some disadvantages, including bleeding in the postoperative period and scar formation.
Stages of the operation:
- insertion of a speculum into the vagina;
- removing vaginal discharge with a cotton swab;
- disinfection surgical field Lugol's solution;
- injections of an anesthetic mixed with adrenaline to reduce bleeding;
- use an electrode loop to cut out the affected area, capturing 3-5 mm of healthy tissue at the edges and 5 mm in depth;
- the removed tissue section is sent to the laboratory for examination;
- To stop bleeding, coagulation of bleeding vessels is carried out.
The duration of the procedure is approximately 15 minutes.
Among the disadvantages of electroconization, it should be noted that it is not always possible to completely remove the pathological area, as a result of which a relapse of the disease is possible.
After the procedure
After the intervention, the patient should remain in the room for about two hours. If there are no significant complaints, the doctor may send her home.
The postoperative period after conization of the cervix may be accompanied by the following symptoms, which are the norm:
- presence of pain aching character lower abdomen;
- slight discharge mixed with blood. There may be an unpleasant odor;
- the duration of discharge may vary: from a week to a month;
- The first menstruation after conization may be heavy.
How does healing proceed after conization of the cervix

If the postoperative period proceeds without complications, then regeneration of the cervix occurs quickly. On days 7-10, the scab formed as a result of coagulation of blood vessels separates, after which epithelization of the wound surface begins. Final tissue regeneration occurs by the 3rd or 4th month.
At the time of healing, a follow-up examination of the woman by a gynecologist is scheduled. If the patient has any complaints, she should visit the doctor ahead of schedule.
Points that should alert you are always discussed and the woman knows what symptoms to pay attention to:
- the appearance of heavy bleeding;
- if your body temperature has increased;
- continuous discharge for more than 4 weeks;
- if there is discomfort in the vagina in the form of burning or itching;
- the appearance of pain in the lower abdomen some time after the intervention;
- increased discharge after it has stopped.
If necessary, carried out local treatment. Suppositories or douching may be prescribed. As a rule, no other additional effects on the cervical mucosa are required during this period.
After 3-4 months, and then every six months after conization, smears are taken to check for the presence of atypical cells. In the absence of pathology for three years, an annual medical examination is indicated.
Restrictions
In the postoperative period, it is necessary to minimize any impact on the cervix. Therefore, the patient will need to introduce some prohibitions:
- Avoid sexual contact for a month;
- do not use vaginal tampons;
- use a shower rather than a bath;
- lifting weights of more than three kilograms;
- refusal to visit the bathhouse and sauna;
- do not overheat;
- Avoid taking blood thinning medications.
Complications
At modern techniques Conization complications are extremely rare. In approximately 1-2% of cases the following may be observed:
- bleeding;
- development of the inflammatory process;
- the appearance of rough scars on the neck;
- lack of ability to bear a child;
- violation menstrual cycle;
- endometriosis.
Pathological changes in the structure of the epithelium of the pharynx of the cervical canal are subject to mandatory treatment in order to avoid complications that are dangerous to the woman’s life. For this purpose, a special operation is carried out - conization.
What it is? Conization of the cervix is a procedure for removing part of the external pharynx, on which there are foci of pathologically altered tissue. The excision is made in the form of a cone: its base is the outer layer of the epithelium, and the apex goes deep into the cervical canal.
The operation allows for complete removal of the affected tissue with relatively shallow tumor invasion.
Indications for the procedure
There must be serious reasons for excision. Conization is not prescribed to patients with ordinary erosion, which responds well to treatment by cauterization, freezing or radio wave exposure. Surgery is performed for a number of reasons:
Cervical dysplasia. The condition is considered precancerous, so it is important to remove part of the organ, including healthy tissue. This is necessary in order to verify through histological examination that the focus of pathologically altered cells is completely excised.
The procedure can be prescribed at any stage of precancerous changes in the structure of the mucous membranes, but conization of the cervix is mandatory for grade 2 and 3 dysplasia.
Areas are pathological altered epithelium with spread into the cervix. In some cases, biopsy results may reveal the presence of atypical cells of unknown origin.
They are not yet a precancerous condition, but the gynecologist cannot guarantee that the focus of altered tissue will not become malignant. An even greater danger is the situation when the focus of atypical cells is extensive.
Malignant formation in the upper layers of the cervical epithelium. This is a borderline state of transition from grade 3 dysplasia to cancer.
Cysts and polyps, located inside the cervical canal and posing a threat to a woman’s health.
Conization is carried out in the first phase of the cycle, shortly after the end of menstrual bleeding. This allows the wound surface formed after surgery to heal before the next menstruation.
Methods of conization, features

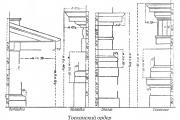
Loop electroconization, photo diagram
Excision of affected areas located on the mucous membrane of the cervix is always carried out according to the same principle. But the methods of surgical intervention are different. For a long time Only one technique was available to surgeons - knife conization.
But now, thanks to the invention of specialized equipment, the number of methods and techniques for carrying out conization has increased: removal of a cone-shaped fragment of the cervix can be done using a laser, radio wave, and loop electroconization.
The attending physician will choose the method that turns out to be the most optimal for a given clinical picture.
Knife conization
- Medical instruments: surgical scalpel;
- Method of anesthesia: general or epidural;
- Indications for use: grade 3 dysplasia, preinvasive and microinvasive (small germination) cervical cancer.
Manipulation
1. The cervix is treated with an iodine solution using a tampon so that the surgeon can see areas of pathologically altered epithelium (they will have a whitish color). Before the operation, an extended colposcopy will be performed.
2. The cervix is fixed with forceps on both sides and brought down. In some cases, the surgeon fixes it with special sutures so that it does not move during the operation.
3. Using a scalpel, the doctor begins to excise a cone-shaped fragment of the cervix. First, the scalpel is immersed to a depth of several millimeters and an incision is made in a circle. The center of the circle is the os of the cervical canal. Then the incised tissue is lifted and fixed in the center using forceps.
The surgeon begins to deepen the incision and once again draws a circle with a scalpel, but with a smaller diameter compared to the previous one. The procedure is repeated until an entire cone-shaped piece of tissue is cut out from the cervix. Since knife conization is indicated for severe lesions, then high excision is usually used.
4. The edges of the wound are coagulated to prevent excessive bleeding and speed up the healing process of the wound surface. Excess blood is removed using a cotton pad.
The knife conization method is considered the most traumatic - it leaves scars on the cervix. They try not to use it to treat women who want to have children in the future.
Radio wave conization
- Medical instruments: Surgitron device;
- Method of anesthesia: regional or general anesthesia;
- Indications for use: pathological changes in the structure of the epithelium, dysplasia of 2 or 3 degrees.
Manipulation
1. In addition to local anesthesia, before radio wave conization of the cervix, treatment is carried out with a special gel containing an anesthetic. Then it is stained with iodine solution to highlight foci of pathology.
2. The surgeon inserts speculum into the vagina, the cervix is fixed with forceps by the front lip so that this area does not enter the surgical area. Mucus is first removed from the cervical canal.
3. The doctor inserts the conizer into the cervical canal to the internal uterine os. Sets the Surgitron device in the “cut and coagulation” mode, and then selects the required power with which it will work. After this, the conizer is rotated once around its axis, and then removed from the cervix along with the excised cone-shaped fragment of tissue.
4. Blood stains are eliminated with the help of a tampon, and the edges of the wound are coagulated, which provokes a narrowing of the radio wave incision made.
If foci of pathologically altered epithelium extend beyond the excision area, then additional rotation of the conizer is performed so that the removed area is wide enough and contains not only malignant cells, but also healthy tissue.
Undoubted dignity radio wave conization is that it is suitable for women who later want to have a child.
Laser conization
- Medical instruments: CO2 laser 10.6 micron laser;
- Method of anesthesia: local;
- Indications for use: dysplasia of the external os of the cervix of the 2nd and 3rd degree.
Manipulation
1. The affected area of the cervical pharynx is marked with Lugol’s solution, and all cervical fluid is removed. The doctor produces local anesthesia, cutting around the area of the proposed surgical intervention from all sides in a circle.
2. A colposcope with a laser device is inserted into the vagina. The part of the cervix that is to be excised is fixed with a tissue clamping instrument. Vaporization (evaporation) is carried out sequentially, along a circle, the center of which is the entrance to the cervical cavity.
With each new circle, the laser beam gradually goes deeper into the tissue; the cut-off area can rise and move away as it rotates.
After cutting off the cone-shaped fragment, the edges of the wound are soldered together. There is an alternative performance of this operation, when the part of the cervix to be removed is evaporated using a laser (destruction). But then there is no material left for histological examination.
3. After the cone is formed, laser resurfacing is performed to smooth out the edges of the wound. Bloody discharge are insignificant, their excess is removed using tampons. Upon completion of the work, the cervix is treated with brilliant green.
Loop electroconization (LLETZ)
- Medical instruments: active electrode with a loop of various shapes;
- Method of anesthesia: local, using Lidocaine or Novocaine;
- Indications for use: dysplasia 2 and 3 degrees
Manipulation
1. The cervix is treated with Lugol’s solution, then the doctor performs an extended colposcopy. The electrode loop is selected according to the examination results so that it can cover the entire affected area. A passive electrode is placed under the patient's buttocks.
2. The cervix is fixed using forceps. To perform a cone-shaped excision, the doctor rotates the electrode around its axis so that the entire area of the pathologically altered epithelium fits into the outlined circle.
With a lesion average size excision must be carried out in one round. If the damage to the external os of the cervix is extensive, the surgeon may make several rounds to completely remove the tissue fragment.
3. After excision, the surgeon treats the wound edges with coagulation to stop bleeding. If the discharge is abundant, then curettage of the cervical canal is performed.
Recovery after surgery occurs in different ways, as does the healing period during conization of the cervix - it all depends on the method by which the affected areas of the mucous membrane were excised.
Knife conization– restoration of the integrity of the mucous membranes occurs after about 2 months. During the first 3 weeks the patient will experience painful sensations in the lower abdomen, which may worsen with prolonged walking or climbing stairs.
During this time, douching, tampons, and sexual intercourse should be avoided to prevent infectious lesion wounds.
Radio wave conization– healing of the wound surface occurs within a month. In the first weeks, when examining the cervix, swelling will be observed. This excision method involves the formation of a scab after conization of the cervix.
After 7–12 days, the scab comes out on its own, causing bleeding.
Laser conization– healing of the cervix occurs after 4 weeks. Serous bleeding will occur within 10-15 days, which is normal. Spontaneous bleeding may occur during the postoperative period.
Loop conization– wound healing occurs after 4-5 weeks. In the first days after excision, quite intense bleeding may be observed, especially if the affected area was extensive and curettage was performed.
Postoperative complications

The postoperative period of cervical conization can be burdened with various kinds of complications. They arise for several reasons: poor-quality excision, failure to comply with aseptic standards during the procedure, or failure to comply with hygiene standards and medical prescriptions by the patient herself after surgery.
- Bleeding from the cervical canal;
- Emergence purulent abscesses on the wound surface;
- Stenosis (narrowing of the lumen) of the cervical canal;
- Hydrorrhea (profuse, long-lasting watery discharge);
- Relapses of cervical dysplasia.
Contraindications to conization
- Inflammation of the cervix of various etiologies.
- Invasive cervical cancer.
- Pregnancy.
- Lactation.
- Menstrual bleeding.
- Ruptures and deformation of the cervix.
- Lack of visualization of the border zone pathological changes epithelium (with laser excision).
Pregnancy after cervical conization
When determining the method by which the affected area will be excised, the doctor must first find out whether the woman is planning a pregnancy in the future.
If the patient’s response is positive, then the least traumatic method of performing the operation is chosen, because pregnancy and childbirth after conization of the cervix are associated with certain difficulties, the main of which is isthmic-cervical insufficiency.
As the period increases, the cervical canal will open under the weight of the fetus, so such patients should be given increased attention The doctor who suggests suturing the cervix or an obstetric pessary will prescribe the exclusion of any physical activity, and in some cases - semi-bed rest.
Conization of the cervix is effective method treatment of malignant changes in the structure of the epithelium of the external pharynx. If the disease is detected on time, the woman has a good chance of being cured and maintaining reproductive functions after surgery.
Cervical diseases in modern ecology are quite common among the female population of most countries of the world. The consequences of treatment for such a pathology, for example, menstruation after conization of the cervix, are of great interest to practicing doctors and their patients.
For successful recovery after radical treatment it's important to imagine possible consequences of this intervention. The rehabilitation period largely depends on the gynecologist’s choice of method of influencing the diseased organ.
Most often, after the operation, a woman is bothered by nagging pain in the lower abdomen. Similar symptoms can last up to 2 - 3 weeks. Experts recommend that their patients take painkillers at this time.
As for the onset of the next menstruation, the surgical intervention performed does not affect their order. Menstrual bleeding usually occurs at the right time, but its intensity can be more pronounced. Many women are forced to take iron supplements during this period to compensate for blood loss.
The color of menstruation in patients who have undergone conization is usually more saturated, discharge dark brown and a peculiar smell. Similar symptoms are caused by areas of coagulated tissue in the cervix.
Such manifestations should not frighten patients, however, if there is heavy bleeding You should consult a doctor. Heavy discharge Blood during the first menstruation after surgery can usually occur in 3% of women, but caution in this case will not hurt.

This method of treating pathology of the female genital area ranks second in the total number of operations performed in this group of patients. In modern clinics, for surgical intervention in such an intimate and delicate place, a special electrode is used - a pan-European type conizer, modified by obstetrician-gynecologist S. Rogovenko.
The essence of the treatment method under consideration is that with the help of this electric knife, damaged tissue of the cervix is excised with a cone-shaped incision, with the sharp side usually facing the inside of the uterine cavity. The resulting stump coagulates and a scab forms in its place, which disappears after some time.
It is the depth of tissue damage by the electrode and the rate of death of coagulated tissue that determines when the first menstruation begins after conization of the cervix.
Diathermoelectroconization is widely used for differential diagnosis of pathology in the vagina and cervix. Using electrodes, a so-called conization biopsy is performed, which, thanks to the morphological picture of a layer-by-layer section of cervical tissue, makes it possible to make a final diagnosis and prescribe appropriate therapy to the sick woman.
Don't go into everything technical details conducting DEE in patients, since such things are of interest mainly only to specialists. It should be noted that this operation is performed without anesthesia, in in rare cases Local administration of novocaine or bupivocaine is recommended.
For 10 - 15
days after conization, women usually complain to their doctor about heavy bleeding from the vagina. A similar picture may persist until the scab is completely rejected from the vaginal cavity.
Serous and bloody discharge during this period are considered common; they are not classified as pathological course postoperative period, and they do not cause concern among specialists.
The doctor should warn the patient before performing the procedure that heavy periods after conization of the cervix should not frighten her. This is how the patient’s body reacts to surgery. Over time, if there are no complications, the volume of menstrual blood secreted will gradually return to the normal preoperative level.
It should be noted that modern gynecology clearly divides all complications of this operation into three main groups according to the time of their occurrence.
The time period for the development of disorders of the female genital organs associated with conization is 3–5 months from the date of surgery. Most often this includes various bleeding from the vagina during intervention or as a result of early rejection of the scab.
This group of patients may develop an inflammatory process in the area of the uterus and appendages. Such complications occur in 1 - 3% of operated women.
Openings with the menstrual cycle are most often simply provoked by the operation performed, however, experts attribute hyperpolymenorrhea and various acyclic bleeding to the consequences of cervical excision. If a woman’s period begins earlier after conization of the cervix, then most often this is a consequence of the manipulation.
If more than 6 months have passed since the operation, doctors usually talk about late complications this medical procedure. These include:
- Shortening of the length of the cervix, accompanied by prolapse of the cervical canal mucosa.
- In 5 - 7% of cases, patients after such an operation develop a sharp narrowing of the cervical canal. Such a pathology requires surgical increase in diameter using special expanders. This is necessary to normalize the release of blood from the uterus during menstruation.
- Inflammatory processes that arise at the site of surgery are possible. Cervical endometriosis and pseudo-erosions of this area are distinguished. A similar pathology has been described in 12–18% of patients after conization.
Many problems in the operated organ are associated with individual characteristics female body and his reaction to such interference.
There are also a large number of long-term consequences of such manipulation, but this is a topic for another discussion. Let us only note that various options Disorders of the ovarian-menstrual cycle are possible in every 6 women who have undergone DEE.
In addition to various complications associated with the development of the inflammatory process in the area of the operation, many patients are concerned possible violations menstruation in the postoperative period. Most often, such problems arise in the first 2 to 3 months after surgery.
When a woman begins her period after conization of the cervix, she will definitely pay attention to their excessive abundance. This is due to the restructuring of work hormonal system and local hemostatic reactions of her body.
After rejection of the scab for 2 - 3 months, the patient undergoes the process of epithelization after excision of the neck. From duration recovery period and the length of time of menstrual irregularities depends.
IN long term Difficulties with menstruation may arise if the cervix sharply decreases in diameter as a result of postoperative spasm. Menstrual blood does not receive sufficient exit from the uterine cavity and can lead to the development of an inflammatory process. To prevent such complications, specialists resort to bougienage of the cervical canal.
According to modern medical statistics, problems with menstruation after such operations are recorded in 20% of patients, and it is noted that these disorders, as a rule, are temporary.
If after conization the patient develops early bleeding, then the actions of health workers depend on its strength and duration. Heavy bleeding require additional hemostasis using DEC with minimal current or various local hemostatic procedures.
Tampons with hydrogen peroxide, adrenaline or aminocaproic acid help well with such problems. A 3% warm solution of hydrogen peroxide is also recommended in the form of baths; cauterization of the bleeding surface with potassium permanganate is indicated.
If necessary, surgical stopping of bleeding is possible. In this case, the cervix is sutured or coagulated using a laser.
Heavy periods that occur after such manipulation in most cases do not require specific treatment, since they wear temporary and functional character. If there is a threat of a critical drop in red blood counts, appropriate symptomatic therapy is carried out.
We recommend reading the article about cervical dysplasia. From it you will learn about the causes of pathology and its diagnosis, treatment methods, the effectiveness of conservative and surgical therapy, as well as the recovery of the body after treatment.
As mentioned above, menstrual disorder after conization of the cervix occurs in only 20% of patients. According to this indicator, diathermoelectroconization is one of the most gentle methods of treating pathological changes in the tissues and cells of this organ, which is problematic for most women. However, when long periods, as well as other alarming symptoms, it is better to consult a doctor.

Nabothian cysts cervixuterus. Neckuterus- a small section of the organ, which is the transition from it to the vagina. .
Periodafterconizationcervixuterus. Why.

Periodafterconizationcervixuterus. Why. .
After biopsy cervixuterusperiod started on time, but their period is longer. It's already the tenth day.

Options as they go periodafter cancellation OK. Oral contraceptives(OK) is one of the popular and effective methods of contraception among women.

Periodafterconizationcervixuterus. why did they start? Periodafter performing a biopsy. Tampons with mumiyo: application in gynecology, how to do it.

Periodafterconizationcervixuterus. why did they start? Signs and treatment of endometrial hyperplasia in menopause. Cervical ectopia cervixuterus with chronic

Especially not performed the day before or during menstruation any operations on cervixuterus. since the discharge will contribute .
Myoma during menstruation | Periodafter operations. What can interfere with the surgeon during menstruation.
A woman's uterus is quite often exposed to the effects of of various nature. As a result of this, various lesions may occur: deformations, ectropion, ruptures after childbirth, benign diseases, cervical dysplasia.
Cervical conization is used to diagnose and treat these lesions.
Features of the procedure
This is a procedure in which a cone-shaped fragment is removed from the cervix. After this, it is sent for histological examination.
There are contraindications for cervical conization:
- diseases of the female reproductive system that are inflammatory or infectious in nature,
- invasive cervical cancer, which is confirmed by the results of histological examination.
Methods of carrying out
Conization of the cervix is carried out in several ways:
- knife using a scalpel, today is practically not used due to large quantity complications, complications
- laser - the most expensive method, inferior in capabilities to the loop method,
- loopback - involves the use of a device radio wave surgery, is the most common.
Conization of the cervix is performed in the first days of the menstrual cycle. At this time, you can be sure that the patient is not pregnant, and in this case there is enough time for the wound to partially heal.
Consequences
After performing conization of the cervix, various complications may occur:
- vaginal bleeding,
- infection,
- narrowing of the cervical canal or external pharynx, which in the future can cause infertility,
- during pregnancy – isthmic-cervical insufficiency,
- prolonged bleeding,
- premature birth.
To avoid negative consequences, in the period after conization of the uterine cervix, several rules should be followed:
- exclude intimacy within one month,
- avoid lifting heavy objects,
- limit physical exercise
- It is not recommended to take baths, go to the sauna, douche,
- do not use tampons,
- do not take medications that may cause bleeding.
After conization of the cervix, some phenomena that are considered normal may be observed:
- spotting for ten days,
- abundant brown discharge With unpleasant smell within three weeks,
- pain in the lower abdomen,
- heavy menstruation in the first months after conization of the cervix.
After conization of the cervix, as a rule, cytological analysis and colposcopy are performed. It is recommended to do this every year. The healing process may take several months. In the future, you need to monitor your condition and regularly visit a gynecologist.
When planning a pregnancy after conization of the cervix, you need to take into account some features. Since a scar forms on the cervix, it may not withstand the load, resulting in a threat premature birth. If the doctor sees this, a suture is placed on the cervix, which prevents premature opening of the uterus. It is removed before childbirth, which is carried out using caesarean section. This is associated with the risk of decreased elasticity of the surface of the uterus, which leads to difficulties with dilatation. During the entire period of pregnancy, you should constantly be under the supervision of a doctor.
Conization of the cervix, which was performed several times in a row, can cause miscarriages on early stages, inability to conceive a child. However, to combat diseases that may develop into cancerous tumor As a rule, one procedure is sufficient.
Dangerous complications
You should immediately consult a doctor in the following cases:
- bleeding is heavier than normal menstruation,
- copious discharge or a lot of clots,
- severe pain in the lower abdomen,
- increased body temperature,
- discharge with an unpleasant odor continues for more than three weeks after the procedure.
If you are reading this material, you are probably about to undergo cervical conization surgery. You've probably already visited the forums asking where and who is the best place to do it - at Herzen, at Blokhin or at Kashirka.
Despite all the doctors’ assurances of the absolute safety of the procedure, conization is a full-fledged surgical intervention, which has very definite consequences for your health.
Unlike the kidneys, ovaries and lungs, the uterus is an unpaired organ. Like the heart, it cannot be replaced, and disruption of the uterus has irreversible consequences.
Therefore, when deciding whether to undergo conization, it makes sense to form an objective opinion about the procedure and find out about alternative effective methods treatment and make an informed decision.
I consciously and responsibly, based on my own practical experience and the clinical data of my patients, declare: even if there are direct indications, in 98% of cases conization MAY NOT BE DONE.
Unfortunately, when offering conization, doctors hide from their patients long-term consequences this procedure. This has been customary in Russian medicine since Soviet times, when even the diagnosis is communicated only to the relatives of the sick person.
2. Relapse. Conization does not protect against recurrence of the underlying disease.
3. Progression of the disease. In 50-70% of cases, within 6-24 months the course of the disease follows a pessimistic scenario and enters a more severe stage.
- Often re-conization is not possible. Each woman has an individual anatomy of the cervix, and not everyone can undergo a second conization after the first conization, even if there are indications. In this case classical medicine can only suggest amputation of the cervix or entire uterus.
Young women come to see me every day, often having not even partially fulfilled their reproductive function, “wound up” about the outcome of the disease, with a strong recommendation from their attending physicians immediately remove the uterus.
Here is one example - the first letter from my patient from Yekaterinburg, now healthy:
“Please tell me, is PDT used in the treatment of CIN 2-3 of the cervical canal? In June 2017, conization was performed at the Yekaterinburg Oncology Center, but dysplasia remained alive in cervical canal, and in its upper part. My attending physician says that they also use PDT, but this is not my case, the uterus must be removed... HPV virus We also treat, but to no avail...”
My dears, dysplasia and other precancerous conditions of the cervix and uterus are successfully treated using photodynamic therapy. Unfortunately, not all specialists are competent enough and strictly adhere to work regulations in the process of preparing and performing PDT.
Therefore, before planning treatment, I have to engage in psychotherapy and restore a method discredited by colleagues.
The conization procedure occupies a special place in the lives of nulliparous women.
Unlike conization, PDT is a non-traumatic therapeutic method. It targets neoplasia in two directions at once:
- destroys tumor and virus-infected cells,
- destroys the papilloma virus in the mucous membranes of the cervix and cervical canal.
By using PDT for treatment, we preserve the integrity of the cervix and uterus and restore immunity at the organ level. Healthy cervix reliably protects itself and the uterus from infections, it is ready for conception, for full independent pregnancy and childbirth.