01.05.2019
Tests before surgery. Complete, or total, endoprosthetics. Contraindications for surgery
In what situations is hip replacement performed? When and to whom? Indications for hip replacement.
Hip replacement surgery is used for the following diseases, injuries and their consequences.
In addition, there is also, which is formed as a result of injury (a fracture in the hip joint that has not healed properly).
Arthrosis can occur as a result, which is characterized by the death of part of the bone tissue of the femoral head.
During total hip replacement surgery, damaged articular surfaces are replaced with biocompatible structures that provide smooth and painless movement in the joint. Your surgeon will do everything possible to return your hip joint to close to its original function. You should discuss with your surgeon what results you can expect in your case.
|
Normal hip joint
On an x-ray of a normal hip joint, articular cartilage (labeled "normal joint space" in the image) is clearly visible as the space between the bony articular surfaces.
|
Hip joint affected by arthrosis
The joint space is noticeably narrowed, causing the femoral head (the ball at the top of the femur) to be in direct contact with the bone of the acetabulum, a condition called bone-on-bone.
|
Total hip replacement
Implants fixed inside the femur and acetabulum,form a new ball-and-socket joint, the components of which are held in contact by muscles and surrounding soft tissue. Implanted structures can be attached to the bone thanks to cement or the special texture of the implant surface into which the bone tissue grows.
|
How is hip replacement performed?
Hip replacement: video 1.
Hip replacement: video 2.
You can learn more about the anatomy of the hip joint (click to go to anatomy article).
Please read this information carefully with your family members. hip replacement.
You will get better results if you read and discuss this guide with your family before surgery.
The team of the clinic of traumatology, orthopedics and joint pathology of the First Moscow Medical University. THEM. Sechenova will make every effort to return to you and your hip joint all the joy of painless movement, as well as to make your stay in the hospital the most useful, educational and, if possible, comfortable. Please feel free to ask questions or seek assistance from any member of staff. medical personnel clinics.
Preparing for surgery
Preparation for total hip replacement begins several weeks before the operation itself. To begin with you will have to:
. Examination before hospitalization. It includes an examination by a doctor, x-rays and a number of tests (blood tests, etc.) necessary to prepare for hip replacement surgery. When you are admitted to the clinic for surgery, based on the results and preoperative examination, you will discuss with your anesthesiologist the type of anesthesia (pain relief) you choose. You can learn more about the preoperative examination accepted in the clinic of traumatology and orthopedics from (click the mouse to go to the article on preoperative examination).
. Medical clearance for surgery: Everything needs to be assessed before surgery. accompanying illnesses(If there are any). Your GP or family doctor can provide invaluable assistance with this. This examination, together with the examination before hospitalization, is necessary to fully evaluate your health and identify conditions that may affect the course of the operation and recovery. If necessary, we can organize your examination in our clinic, but it is preferable to carry out the examination on an outpatient basis.
If you have arterial hypertension (hypertension, characterized by increased blood pressure), then if the pressure numbers “jump”, i.e. treatment regimen arterial hypertension is inadequate, before a planned operation it is advisable to adjust the treatment by selecting the drugs you need according to correct dosage. If the therapist prescribes you any drugs that affect blood clotting, be sure to inform your doctor about this.
If you have diabetes, then before the operation it is also necessary to compensate for it, i.e. reach normal content blood sugar by selecting a diet, hypoglycemic drugs.
If you have any other chronic disease that requires treatment, be sure to optimize your treatment regimen with your doctor based on the profile of this disease. Do not forget to inform your attending physician at the traumatology and orthopedics clinic about any concomitant disease.
What else needs to be done in preparation for endoprosthetics:
. Start training under the supervision of a doctor: this is necessary so that during the operation you are in the best possible condition physical fitness. Special exercises will allow you to strengthen the muscles of your torso and arms, which will make it easier for you to use crutches and walkers in the first days after surgery in the postoperative period, and exercises that strengthen the muscles of your legs will reduce the time required to recover after surgery.
. Practice walking on crutches: the existing skill of walking on crutches will help you recover faster, because you will begin to get up and start walking the next day after the operation. You can buy crutches or rent them.
. Control your weight: If you are overweight, then losing weight will help reduce the load on the endoprosthesis. If your weight is within normal limits. just keep it stable. We understand that sometimes losing weight is simply not possible because hip pain interferes with the physical activity needed to achieve a healthy body weight. After hip replacement, the pain will go away and then the task of losing weight will become easier. Please continue to work in this direction - in this case, the load on the endoprosthesis will be less and it will last longer.
. Consider donating your blood for transfusion during surgery: If your surgeon thinks you may need a blood transfusion, you can donate your blood in advance to be given during surgery.
. Visit the dentist: Although infectious complications They occur infrequently during joint replacement; they can develop if there is an infection somewhere in the body and bacteria can enter the bloodstream. Therefore, you must complete all dental procedures, such as caries treatment, prosthetics and dental fillings, even before surgery. If you need extensive treatment for dental problems, you can postpone them and return to dental treatment one year after hip replacement.
. Stop taking certain medications: Your surgeon will tell you which medications you need to stop taking before surgery. Tell your surgeon about all the medications you take, including over-the-counter medications, as some may increase bleeding during surgery. It is important to note that taking aspirin medications (trobo-ass, etc.) does not interfere with endoprosthetics and they do not need to be discontinued.
. Stop smoking:uh This is a good thing to do at any time, but quitting smoking is especially helpful before major surgery to reduce the risk of post-operative lung problems, improve healing, and reduce the risk of complications.
. Assess your needs for home care after discharge from the hospital:
Most hip replacement patients will need home care for the first few weeks, including assistance with cooking and moving around the house.
After reading this information, everything may seem very complicated to you.Don't worry, we actually try to warn you about all the features, even those that may be unnecessary. For example, many patients after hip replacement can walk without any problems after just a couple of weeks, using only one crutch. In any case, in this article we try to describe the entire process as fully as possible, to create a kind of “school” of endoprosthetics. And you, being armed with knowledge, will be able to defeat the disease much easier with our help.
About blood transfusion
A patient may need a blood transfusion during hip replacement surgery. It is worth discussing this issue with your surgeon. If you are a candidate for a transfusion, you have several options:
Autogenous transfusion. Autogenous blood transfusion is a method where you donate your own blood in advance. If necessary, doctors will tell you how to donate blood at a Blood Transfusion Center or another institution. The process is extremely reliable and your blood can be safely frozen for at least a month. The obvious advantage of this option is that when using your own blood, there is absolutely no risk of contracting blood-borne infections.
Homologous transfusion. Homologous transfusion is a blood transfusion from another donor. This is usually the blood of an unknown person who donated blood (donor), but family members and friends whose blood is suitable for you have the opportunity to donate blood specifically for you. Regardless of origin, all homologous blood is tested by the blood bank for blood-borne infections.
Preparing your home
Things you can do at home before you go to the hospital for surgery to make it more comfortable and safe when you return:
- In the kitchen and other places, place items you use regularly at hand level so that you don't have to reach or bend over for them.
- Buy a cordless phone if you don't already have one.
- If you live in a separate house, consider avoiding unnecessary stairs by changing the purpose of the rooms - for example, temporarily turning the living room into a bedroom.
- Rearrange furniture to give yourself enough space to walk with crutches or a walker.
- Get a suitable chair - one that is sturdy, with a seat high enough so that your knees are lower than your hip joints, and with secure armrests to make it easier to get up from.
- Remove rugs and electrical cords from areas where you will walk. To make it easier to move around after you are discharged from the hospital after surgery, walk around your apartment or home with your family as a "sleuth" or safety specialist: remove or double-sided tape the corners of any rugs that ride up to prevent tripping hazards. . Remove loose wires on the floor. If you have parquet at home, check its planks so that none of them fall out. Imagine that a “child” should appear in your house in terms of moving around the apartment: plan it so that there is something to hold on to (but the support should be stable, not a plastic shelf) and there is nothing to trip over. Cover the sharp corners of tables and other furniture with special soft pads (sold in children's stores). Ensure normal lighting in all rooms and corners of your home.
- A small stool will be useful as a support for your operated leg to keep it straight in front of you when you sit in a chair.
- Find a matching shirt or vest with large pockets, or a soft shoulder bag to carry small items.
- Set up a “recovery center” in your home: with a telephone, TV, remote controls, radio, cosmetic wipes, a jug, a glass, magazines and books, as well as medicines within arm’s reach: sometimes you just want to relax and not torment yourself with unnecessary getting up and walking.
- If you have pets that can push you or get under your feet, it is best to give them to relatives, friends or keep your pet in a kennel for a few weeks, because if your pet pushes you, you may fall and damage your new joint .
Place soap, shampoo and other bath items so you don't have to turn around or reach to get them.
Day before surgery
As a rule, we set a date for hospitalization at the Traumatology and Orthopedics Clinic of the First Moscow Medical University named after. THEM. Sechenov in such a way that the operation could be performed the next day.
Please arrive at the clinic between 10.00 and 14.00 on the day of hospitalization, unless your attending physician tells you a different time.
What to take with you to the hospital and what not to take?

|

|
|
Toiletries ( Toothbrush etc.).
Your cane or crutches.
Shoes (outdoor and slippers). It should be stable, with a heel no higher than 3 centimeters. Please ensure that both outdoor shoes and slippers have non-slip soles. Slippers should not have excessive decorations, wool, fur or down decorative elements. Shoes should be easy to put on and take off.
A short nightgown, loose pajamas, or loose shorts that can be worn over the headband.
Lightweight, not too long bathrobe.
Veet type epilation cream.
Cellular telephone and charger.
Glasses instead of contact lenses - they require no maintenance and are more difficult to lose.
A list of your medications, including those you recently stopped using as recommended by your surgeon. If you are taking any customized medications for another condition, take them with you.
A small amount of cash - to purchase a newspaper, pay for a telephone, etc.
A book, a magazine, something that will help pass the time and distract you.
You can take your laptop or DVD player with you.
Internet access in the clinic is possible via GPRS modems or Yota modems.
If you have dentures/hearing aids, bring them with a storage container.
Print this article and take it with you.
|
Jewelry, large sums of cash, credit cards (except essential), wallet, watch.
All hospital staff respect your property rights, but we cannot guarantee the security of your personal property because the hospital is a public place.
|
After you arrive at the clinic, your attending physician will check the results of preoperative tests and studies, review your comorbidities again, and make a final decision about hospitalization.
Next, documents are drawn up (agreement on the provision of medical care within the framework of voluntary health insurance or for a fee). If endoprosthetics is carried out at the expense of the federal budget (as part of high-tech medical care, i.e. according to a “quota”), then all documents must be completed earlier.
Then a medical history is taken in the emergency room, and you can be placed in the ward.
On the day of hospitalization, your attending physician will definitely talk with you, who will fill out medical documentation together with you. It will display your medical history, information about your health, primary and concomitant diseases. They will discuss the plan for the upcoming operation with you and inform you about its advantages and disadvantages. This process is called informed consent for treatment. Do not hide any information about your health from your doctor and do not hesitate to ask questions if something is unclear to you or, conversely, you want to know more about something. During the medical history process, you will be asked to fill out a questionnaire that will contain questions about your medical condition. At the end of the conversation with your doctor, you will have to sign an informed consent for treatment.
After this, if necessary, you will be consulted by a therapist or other specialists.
Then an anesthesiologist will come to you, who, after reviewing your medical history, the results of tests and examinations, will discuss with you the chosen anesthesia option. As a rule, regional (spinal) anesthesia or endotracheal anesthesia is used for hip replacement. We'll talk more about anesthesia later.
Diet: On the day before surgery, you can eat as usual, but should not drink alcoholic beverages.
On the day before surgery, do not eat anything after 7 pm or drink anything after midnight.
This is necessary so as not to interfere with normal anesthesia. An exception may be made if your doctor has specifically instructed you to take your medications with a sip of water. Shower the night before or the morning of surgery. In this case, it is advisable to use soap or shower gel with triclosan (Safeguard type soap, etc.). After showering, use clean bedding and underwear.
Anesthesia
Anesthesia is the process of putting you into a sleep-like state in which you will experience no pain or anxiety during surgery. The anesthesiologist has several ways to ensure that your operation is painless and comfortable. Some concomitant diseases or your individual characteristics may make one or another method of anesthesia more preferable. You can discuss these methods with both the surgeon and the anesthesiologist. Whatever method is chosen, you are guaranteed to experience neither fear nor pain in the operating room.
General anesthesia (anesthesia). First, with the help of gaseous drugs that enter your lungs with the air you inhale through the mask, you will be put into a sleep-like state. Next, intubation is carried out, i.e. a special tube is inserted into the airway. This tube is connected to the ventilator. During the operation, your condition will be monitored using sensors connected to you. With their help, the anesthesiologist will constantly monitor your heart rhythm, blood oxygen levels, body temperature and blood pressure. Immediately after the end of the operation, the endotracheal tube is removed, the person wakes up and breathes on his own.
Regional anesthesia. Some patients refuse regional anesthesia because they think they will be awake during surgery. This is not true. During regional anesthesia, you are also given medications to help you sleep peacefully during surgery. Unlike anesthesia, after the regional anesthesia wears off, you will wake up almost immediately and without pain (because the anesthesia will still be in effect). Two types of regional anesthesia are commonly used: spinal and epidural. They can also be used in combination.
On the morning of the operation
You can brush your teeth and rinse your mouth without swallowing water.
Leave valuable property to relatives or give it away for safekeeping.
You will be asked to remove all jewelry except your wedding ring, which may be secured to your finger with adhesive tape. It is best to leave all decorations at home.
If you are using a hairpiece or wig, it must also be removed.
It is necessary to remove polish from fingernails and toes using special nail polish removers.
If you wish, you can ask your surgeon to call your family after the operation is completed.
Before the operation, a compression stocking will be put on the opposite leg or the leg will be bandaged with an elastic bandage up to the knee. This is done to prevent the formation of blood clots.
You will be taken to the operating room on a gurney.
After you have been given anesthesia, a tube (catheter) will be inserted into your bladder. This is necessary for two reasons:
1. While under anesthesia, you are unable to control urination.
2. The doctor needs to monitor the amount of fluid released by your body. Catheters are usually removed on the second day after surgery.
Pre-Surgery Checklist
The night before surgery:
Shower (may be taken on the day of surgery if time permits). After showering, put clean underwear on your body.
If medical personnel have told you to remove hair from your thigh, please do not use a razor, which may cause scratches or abrasions. It is best to use simple epilation creams like “VEET”. If there are scrapes or cuts on the skin, surgery may need to be rescheduled because they may increase the risk of infection.
Do not eat anything after seven o'clock in the evening and do not drink anything after midnight.
Have a good rest tonight. Don't worry and get some sleep. If necessary, you will be given medication the evening before surgery to help you cope with anxiety.
Day of surgery:
Take your medications as usual - with a sip of water, if recommended by your doctor.
Brush your teeth and rinse your mouth - without swallowing water.
Wear comfortable clothes.
Leave valuables with relatives or give them for safekeeping.
After operation
When the operation is completed, you will be moved to the recovery room, where you will stay for two to three hours before being transferred to your permanent ward, where you can see your family and friends. Please, if possible, limit your visits to a minimum circle of people close to you, since your stay in surgical department a large number of strangers can be harmful from the point of view of your infection safety. In addition, the clinic also treats other people who may be disturbed by excessively large delegations of your relatives and friends. Often after surgery, patients are returned directly to their room, without spending time in the recovery room.
Depending on the type of anesthesia, your general health and other factors, you may first be transferred to a ward intensive care or to the postoperative department for a longer period of time. Your surgeon or anesthetist will discuss this with you before surgery. The team of staff providing your medical care will monitor your condition regardless of your location in the hospital, which will ensure your effective and safe recovery. Your body temperature will be periodically measured and your vital signs checked. important functions, arterial pressure, change the bandages covering the area of the surgical wound. Your surgeon may decide to give you a blood transfusion or prescribe medications to thin your blood and prevent blood clots. In addition, antibiotics will be administered for 2-3 days after surgery.
FAQ:
When can I eat? Most patients do not feel hungry immediately after surgery. Patients are usually ready to eat solid food the evening of the day of surgery. Sometimes there is nausea, but it usually goes away quickly. It is important to let your nurse know if you are feeling sick so she can give you medicine to make you feel better. It is better to start eating and drinking after surgery in small sips, a little at a time, with breaks, so as not to provoke nausea.
What happens the day after surgery?
Typically, the bladder catheter is removed within a few days after surgery. You may feel a slight burning sensation for one to two seconds after it is removed.
The next day after the operation, the dressing is done.
Often the operation is completed with drainage - i.e. install a tube through which the wound fluid will be collected in a special container. Removing the drainage does not require any pain relief - as a rule, patients do not even notice that the drainage has been removed and even ask: “Well, when?” Yes, everything has already been deleted.
When can I take a shower?
Your surgeon will insist that you cover the surgical wound area while showering until it has completely healed. You can usually shower without scar protection 24 hours after sutures or staples are removed (10-14 days after surgery). Often, monofilament sutures are used to close the wound, which allows you to shower earlier, even before removing the sutures.
The safest way to shower is while sitting.
Pat dry rather than wipe the surgical scar after showering.
Pain relief after surgery
Many patients are afraid of post-operative pain, and this is understandable. Pain control is currently a very complex process. Usually the level of discomfort is easily regulated with the help of painkillers in the form of tablets or injections.
In some cases, patients receive an epidural or intravenous catheter, which allows the administration of painkillers on demand for several days (type IV-PCA systems, intravenous patient-controlled analgesia, - intravenous, patient-controlled analgesia). You just need to press a button, and a new, safe dose of effective pain relief will enter your body. An epidural (spinal) catheter automatically delivers pain medication.
A team of clinic staff providing you with medical care
. Head of department
Your Therapist
. Nurses
. Physiotherapy doctor, rehabilitation doctor
. Postgraduate students and medical residents. Clinic of Traumatology and Orthopedics of the First Moscow Medical University named after. THEM. Sechenov, the largest medical university in the country, also carries out an educational function. In our clinic, doctors undergo postgraduate training in the specialty “traumatology and orthopedics”. These doctors assist in the treatment process, but they do not make any independent decisions regarding your treatment process.
. Therapist: A medical specialist chosen by your surgeon to provide you with post-operative care.
One or more of our team doctors, depending on your needs, will visit you every day or more often while you are in the hospital.
Physical therapy and exercise
On the first day after surgery, it is better to lie in bed. If any medical procedures are required (for example, control x-rays), you will be transported on a medical gurney.
First of all, your doctor will instruct you about simple rules behavior with a new hip joint. They must be observed starting from the first days of the operation and certainly in the first few months. These are the rules:
Preventing dislocation: right angle rule.
To reduce the risk of endoprosthesis dislocation, you must remember the right angle rule: Do not bend your leg at the hip joint more than ninety degrees (right angle). You should also avoid crossing your legs and squatting.
When you get out of bed, sit only in chairs or armchairs that allow less than ninety degrees of hip flexion.

When you are lying or sitting, try to move your operated leg slightly to the side. To control the correct position of the leg, there is a rule of thumb - place your finger on the outer surface of the thigh and in the correct position the knee should be on the outside of the toe.

When you are lying in bed, do not try to pull the blanket that lies at your feet over yourself. Use any device for this or ask someone to help you.
Likewise, do not wear shoes without a spoon.

Later, as the muscles, ligaments and tendons surrounding your new joint become stronger, you may be able to give up some of these rules, such as the need to place a pillow between your legs at night.
However bed rest on the first day after surgery does not mean that you should not do anything - it’s time to fight for recovery!
Exercises to do immediately after surgery
These exercises are needed to improve blood circulation in your legs and prevent the formation of blood clots (thrombi).
They are also needed to strengthen muscles and improve movement in the hip joint. Don't give up if some exercises don't work out well at first. They will speed up your recovery and reduce post-operative pain. All exercises must be performed SLOWLY.
Not all exercises are suitable for all patients. Your doctor will point out the exercises that are right for you. If you are not given other recommendations, do these exercises three times every day: morning, afternoon and evening.
 |
Foot pump:
When you're lying in bed (or later when you're sitting in a chair), slowly move your feet up and down. Do this exercise several times every 5 or 10 minutes. This exercise can be done either sitting or lying down. You can start doing this exercise immediately after surgery while still in the recovery room. Continue doing this exercise periodically until full recovery.
|

|
Rotation at the ankle joint:
Rotate the foot of the operated leg, first clockwise, then in the opposite direction. Rotation is carried out only through the ankle joint, not the knee! Repeat the exercise 5 times in each direction. It can be performed both sitting and lying down.
|
 |
Exercise for the quadriceps femoris muscle(muscle on the front of the thigh): Tighten the muscle on the front of your thigh (quadriceps). Try to straighten your knee by pressing the back of your leg into the bed. Hold the muscle tense for 5 - 10 seconds.
Repeat this exercise 10 times for each leg (not just the operated one).
|
 |
Knee flexion with heel support:
Move your heel toward your buttocks, bending your knee and touching your heel to the surface of the bed. Don't let your knee rotate toward your other leg and don't flex your hip more than 90 degrees. Repeat this exercise 10 times.
|
 |
If at first it is difficult for you to perform the exercise described above on the first day after surgery, then you can hold off on it. If you continue to have difficulty later, you can use tape or a folded sheet to help tighten your foot.
|
 |
Buttock contractions:
Squeeze your butt muscles and hold them tight for 5 seconds. Repeat the exercise at least 10 times.
|
 |
Abduction exercise:
Move the operated leg to the side as much as possible and return it back. Repeat this exercise 10 times. If at first it is difficult for you to perform this exercise on the first day after surgery, then you can hold off on doing it.
|
 |
Straight leg raise:
Tighten your thigh muscles so that the knee of your leg lying on the bed is fully straightened. After this, raise your leg a few centimeters from the surface of the bed. Repeat this exercise 10 times for each leg (not just the operated one). If at first it is difficult for you to perform this exercise on the first day after surgery, then you can hold off on doing it.
|
Continue these exercises later, on the subsequent second, third, and so on days after hip replacement surgery.
The day after surgery, your doctor or physical therapist will help you stand up and you will begin walking with crutches or a walker using your new hip joint. In most cases, you will be allowed to step on the operated leg with the full weight of your body. This is called weight bearing based on the principle of pain tolerance. Sometimes, due to the nature of your surgery, your surgeon may initially limit the weight on your operated leg, this is called partial weightbearing. After some time, you will be able to increase the load on the operated leg.
Postoperative wound care
Usually the wound is sutured or the edges of the wound are secured with special staples. The sutures are removed 12-14-16 days after surgery.
Sometimes the wound is sutured with absorbable sutures that do not need to be removed.
Until the sutures are removed, it is enough to remove the sticker from the wound once a day (and with normal healing - once every two to three days) and wipe the seam with a clean cloth soaked in saline solution. While you are in the clinic, your dressings will be performed by nurses who, if necessary, will call a doctor to look at the postoperative wound.
After discharge, keep the wound dry and clean.
Tell your doctor if there is redness around the wound or if wound fluid starts to ooze from the wound.
In the first few months after surgery, the operated leg will swell - this is normal and you should not be afraid of it.
Movement after surgery
Walking with a walker or crutches: stand straight up so that you are comfortable. Distribute your weight evenly using a walker or crutches. Move walkers or crutches a short distance. After this, move forward so that the operated leg touches the floor with the heel first.
As you complete your step, allow your big toe to lift off the floor. Again, position your walker or crutches slightly in front of your hips and knees to perform next step. Remember, first touch the floor with your heel, then place your foot on the floor with its entire surface, then lift it off thumb from the floor surface. Try to walk as rhythmically and smoothly as you can, but don't rush. Choose your stride length and speed to move that way.
As your muscle strength and endurance are restored, you will be able to walk more. Gradually you will be able to put more and more weight on the operated leg.
Approximately the third day after surgery
You will be able to walk fairly confidently with the help of crutches or a walker. Most patients are surprised at how independent they become and how quickly it happens.
Walking with a cane or one crutch:A walker is often only used for the first few weeks to help you maintain balance and avoid falls. A cane or one crutch is used for several more weeks until strength and balance are fully restored. Use a cane or crutch in the hand opposite the operated joint. That is, if the right joint was operated on, then keep one crutch under your left arm, and vice versa. You will be ready to walk with a cane or one crutch when you can stand on both feet and maintain your balance without the aid of a walker.
Ascending and descending stairs: Climbing stairs requires both joint mobility and muscle strength, so if possible, it should be avoided until complete recovery. If you have to use stairs, you may need assistance. Always use the hand opposite the operated joint to rest on the railing when climbing stairs and take one step at a time.
Climbing stairs:
1. Step up with your healthy leg.
2. Then move your operated leg up one step.
3. Finally, move your crutch and/or cane to the same step.

Descending the stairs, everything in reverse order:
1. Place your crutch and/or cane on the step below.
2. Take a step down with your operated leg.
3. Finally, move your healthy leg down.
Do not forget that you should always start climbing stairs with a step with your healthy leg, and descending with a step with your operated leg.
Exercises in the early postoperative period
In addition to the exercises already described, which are performed in the first few days after the operation, from the second day after the operation, when you can already stand, exercises in a standing position are added to them.
Soon after surgery you will be able to get out of bed and stand. You will need help at first until you have regained your strength and are able to stand without additional support. When performing these exercises in a standing position, hold on to reliable support (headboard, table, wall or sturdy chair). Repeat each exercise 10 times during each session:
 |
Standing Knee Raise:
Raise the knee of your operated leg. Do not raise your knee above waist level. Hold your leg for two seconds and lower it on the count of three.
|
 |
Straightening the hip joint in a standing position
: Slowly move your operated leg back. Try to keep your back straight. Hold your leg for 2 or 3 seconds, then return it back to the floor.
|
 |
Leg abduction in a standing position:
Make sure your hip, knee, and foot are pointing straight forward. Keep your body straight. Keeping your knee pointed forward at all times, move your leg to the side. Then slowly lower your leg back so that your foot is back on the floor.
|
Typically, after hip replacement, you have to spend 7-10 days in the clinic.
You may be discharged home if:
- Your doctor is confident that you are able to move around and get in and out of bed safely.
- You can reach the bathroom or toilet.
- You are eating solid foods.
- There are no signs of infection in the area of the surgical wound.
- Your vital signs are normal.
- You can control pain with medication tablets.
- Your doctors will find the test results satisfactory.
Upon discharge, you will receive a discharge summary, which will list recommendations for further restoration, the type and size of the endoprosthesis components installed for you are indicated.
If you plan to go home by car or taxi, you should provide a hard cushion on which to sit. A higher seat level will make it easier to get in and out of the car. To make it easier to fit, you can use a plastic bag that will allow it to slide over the seat.
Exercises and activities performed at a later stage
Full recovery will take some time. The pain caused by joint disease before surgery and the surgery itself have weakened your hip muscles. The following exercises will help these muscles fully recover:
 |
Exercises with elastic band (with resistance).
These exercises should be performed in the morning, afternoon and evening 10 times. One end of the elastic band is secured around the ankle of the operated leg, the other end - to a locked door, heavy furniture or wall bars. To maintain balance, you should hold on to a chair or headboard.
|
 |
Hip flexion with resistance:
Stand with your back to a wall or heavy object to which an elastic band is attached, with your operated leg slightly to the side. Raise your leg forward, keeping your knee straight. Then slowly return your leg to the starting position.
|
 |
Leg abduction with resistance in a standing position:
Vstand with your healthy side towards the door or heavy object to which the rubber tube is attached, and move your operated leg to the side. Slowly return your leg to the starting position.
|
Exercises on an exercise bike:
Exercise on an exercise bike is a wonderful exercise that allows you to restore muscle strength and mobility of the hip joint. Adjust the seat height so that you barely touch the pedal with your knee straight. First, pedal backwards. Start pedaling forward only after you can easily pedal backward. As your muscles become stronger (approximately 4-6 weeks after surgery), gradually increase the load.
Remember to follow the right angle rule: do not raise your knee higher than your hip joint.
Pedal forward for 10-15 minutes twice a day, gradually increasing this time to 20-30 minutes 3-4 times a week.
Dislocation. After any hip replacement surgery, there is a risk of dislocation (“popping”) of the endoprosthesis, especially in the first few days and weeks after surgery. Fortunately, this is a complication whose risk you can significantly reduce if you follow the rules and engage in rehabilitation that will strengthen your muscles.
If your endoprosthesis dislocates, the first thing you should do is tell your doctor. Your surgeon will instruct you on how to get immediate help, either at the hospital where you had the operation or at the emergency department of the emergency hospital. Every orthopedic traumatologist knows how to set a dislocated endoprosthesis (return its head to the cup).
To reduce the risk of re-dislocation of the endoprosthesis, your surgeon may recommend wearing a special device, a brace, that limits movement in the hip joint. Although some risk of dislocation always remains, it is greatly reduced once the soft tissue surrounding the joint has healed after approximately 3 months.
Always remember the Right Angle Rule and avoid extreme twisting and flexion of the hip.
Fracture. A fall or injury may result in a fracture of the bone around the endoprosthesis. Treatment of a fracture of envy depends on its character.
Loosening of the implant and its wear. After a standard hip replacement, there is a 90-95% chance that your hip will last more than 10 years. But the endoprosthesis still does not last forever. After some time, signs of wear and tear of the implant may appear, it may become loose, and it may require replacement or revision endoprosthetics. Ongoing research offers hope for increasing the lifespan of implants and making them easier to replace in the future. Feel free to discuss the level of technological advancements with your doctor when discussing implant design.
Total hip replacement: complications
If wear or loosening of the endoprosthesis components occurs, revision endoprosthesis replacement is performed.
Revision hip replacement
Damage to a blood vessel or nerve. With arthroplasty, as with any other operation, there is a risk of damage to nerves or blood vessels, but it is extremely low. The probability of damage to blood vessels and nerves during hip replacement is a fraction of a percent. If you experience sudden numbness or weakness in your leg or foot after surgery, tell your doctor or nurse right away.
Different leg lengths. In patients with arthrosis of the hip joint, the leg on the affected side is often shorter than the other. Although your doctor will try to straighten the length of your legs, this is not always possible or necessary. The vast majority of patients do not note any significant difference. If you notice a difference in leg length and it causes you discomfort, it can be easily eliminated with the help of heel pads or heel caps. Often after surgery, patients feel the operated leg as longer, and this is due to the fact that long time it was shorter, and the muscles and spine got used to the short leg. Typically, the feeling of a long leg goes away over a few weeks or months as the spine, pelvis and muscles become accustomed to the new length of the leg. The sensation of a long leg is often accompanied by pain along the front of the thigh, which will also gradually subside.
Problems with the hip joint have always caused great inconvenience in addition to pain. People with such a disease suffered from unbearable pain, even when they were in a sitting or lying position, the joint made itself felt by its soreness. Doctors have found a way to save people suffering from this disease. Hip replacement is one of the panaceas of modern medicine.
Hip replacement helps people return to normal life without pain. Therefore, when a doctor suggests a hip replacement, you must give consent, because returning to a normal lifestyle without pain is very important.


Hip replacement occurs when certain types injuries, bone diseases, etc. We will consider the most common questions that torment a person when making such a choice here.
In hip replacement, a total prosthesis is very often used. It is also called an implant. This endoprosthesis has two parts - the acetabulum and the epiphysis, which, in turn, completely replace the natural bone parts that require replacement. There are different sizes, so they are personally selected for each patient.
Today, long incisions are not made, which has a beneficial effect on the muscles, in which peeling does not occur, and the soft tissues surrounding the joint do not suffer. The operation is performed using a minimally invasive method.

 An incision is made to the patient at the back approximately at the level of his swimming trunks; it is almost invisible. An experienced surgeon penetrates from behind, without affecting the group of muscles that are important for walking, located on the side of the thigh, and installs the implant. This installation of the prosthesis has a beneficial effect on the restorative function of the hip joint after surgery.
An incision is made to the patient at the back approximately at the level of his swimming trunks; it is almost invisible. An experienced surgeon penetrates from behind, without affecting the group of muscles that are important for walking, located on the side of the thigh, and installs the implant. This installation of the prosthesis has a beneficial effect on the restorative function of the hip joint after surgery.
At the very end of the operation, drainage is done to remove fluid and blood from the wound, then a bandage is applied. Almost immediately, an x-ray is taken, which serves as a kind of control about the manipulation performed and its effectiveness. In the ward, pillows are placed under the operated leg or it is placed in a special splint.
There are cases when, after total hip replacement, it is necessary to undergo revision hip replacement. Why it needs to be done, let's figure it out.
Revision hip replacement
Indications for revision hip arthroplasty may include:
- Loosening of the joint components itself;
- The appearance of pain;
- Old dislocations;
- Impaired walking;
- Suppuration;
- Also, disruption of the installation of the prosthesis during surgery plays an important role;
- The implant itself is made with a defect that can only appear after use;
- Wear of the prosthesis;
- The inflammatory process has begun;
The above reasons influence the mandatory replacement of a prosthesis that has already been installed.
We would like to say the following: not everything can depend on the hands and experience of the surgeon. There are many reasons why revision arthroplasty is necessary. Therefore, before you get upset and scold the doctor, first figure out why this happened.
Preparation for hip replacement
Having agreed to undergo joint replacement surgery, it is necessary to prepare for hip replacement. First, go through a full diagnostic. It is possible that after such an examination chronic diseases will be discovered; they must be cured as much as possible. It is advisable to bring your weight to normal; this will affect the physical load of the joint after surgery. It is advisable to create a supply of your own blood, this is necessary if bleeding occurs. If you can’t donate blood yourself, try to find a donor just in case of emergency. You yourself will be calmer this way.
It is best to prepare for hip replacement at home one month before the scheduled procedure. A series of ways to strengthen and heal the whole body on your own will give in the future positive result during the rehabilitation period. The exercises are simple and if pain haunts you, you just need to limit yourself to the number of times you perform it and reduce the intensity of the load. These rough guidelines will help you talk to your doctor during your pre-surgery consultation.
It is necessary to strengthen the buttocks, legs and back:
- Lie on the floor, at the same time begin to squeeze and unclench your buttocks for a few seconds;
- Lying on the floor, straighten your arms along the length of your body, palms down. Feet stand straight, knees slightly bent. In this position, begin to raise your hips to a small height. Perform 10-20 times if possible;
- Lying on the floor, bend your knees, from this position you need to raise your legs simultaneously to a right angle relative to your body. This is a kind of semi-birch tree. Hold in this position for 3-5 seconds, then slowly lower to the starting position;
- Take a standing pose. Alternately, begin to rotate the ankle to the right 10 times, then to the left 10 times;
Simultaneously with such exercises, you need to start taking medications, preventing the risk of bleeding during and after surgery. will help strengthen the body as a whole.
It is also advisable to contact the insurance company and inform them about the upcoming operation, then find out whether the insurance company can reimburse you for rehabilitation procedures.
Preparing household utensils after surgery
So, the operation is behind us, ahead.
Complications may occur in a short period of time after surgery. Therefore, we will write information about this unpleasant side after the operation.
Here is one of the comments from the forum “...my daughter developed thromboembolism after prosthetics (a high prothrombin index occurred against the background of disseminated intravascular coagulation syndrome). This was dealt with quickly, but the rehabilitation time from this increased slightly.”
Complications are possible, but not necessary, and occur in rare cases. Doctors today are trying to make prosthetics work without complications, and they are succeeding.
Complications
Hip replacement is a very serious operation; it is necessary to notice certain complications in time to avoid problems in the future.
Complications after hip replacement may include:
- Allergic reaction to anesthesia;
- Heart attack;
- Thromboembolism or blood clot formation;
- Infection;
- Dislocation of the installed prosthesis;
- Wear or loosening of the prosthesis;
- Vascular or nerve injury;
- Old fractures of the femoral neck.
Reasons for getting disability
Some people think they will become disabled by having a hip replacement.
In order to understand under what circumstances a disability group is given, let’s consider the grounds for assigning such a group:
- Deforming arthrosis, a combination of moderate dysfunction of joints and no less;
- Deforming osteoarthritis of several joints or one with concomitant shortening of the limb or ankylosis;
- Bilateral endoprosthetics resulted in severe violations.
All of the above regarding the assignment of a disability group can mean one thing: hip replacement surgery serves as a method of treatment. Recommended in the late stage of deforming osteoarthritis.
Disability can only be obtained after complicated bilateral arthroplasty, but this is a big exception.
Hip replacement helps restore its function in 90% of cases. The ability to move independently returns, lameness and pain disappear, and the need to use assistive devices disappears. However, hip replacement is a contraindication to active sports - running, skiing, jumping. The prosthesis has a limited range of movements, but this is enough to improve the quality of life. The service life of the implant is 15 years, after this time it is replaced with a new one.
Currently, there are more than 70 types of prostheses. The success of the operation depends on following the doctor’s instructions and correctness. The patient must know what exercises can be performed and at what time.
Indications and contraindications
Main indications for surgery:
- coxarthrosis;
- underdevelopment of the hip joint;
- arthritis;
- destruction of the femoral head;
- damage to the femoral neck.

Contraindications:
- acute infections;
- significant destruction of bone tissue;
- heart failure;
- allergic reactions to materials used during surgery.
Endoprosthesis technology
Total prosthetics is a complex, high-tech intervention that requires extreme care from the surgeon. Depending on the type of disease, a specific type of prosthesis is selected.
What to do before surgery
How to prepare for endoprosthetics? Preparation for surgery involves examination, including:
- general and biochemical analysis blood;
- electrocardiography;
- X-ray of the joint in several projections.

CT or CT scans can be used to confirm the diagnosis. Patients with chronic diseases must provide permission from a specialist.
10 days before hip replacement, treatment with anticoagulants and some other drugs is stopped. The last meal is taken no later than 8 hours before surgery. Before the intervention, jewelry, contact lenses, and dentures are removed. The operation lasts 2–3 hours. Before it begins, the patient lies on his side and bends the limb, which is fixed to the table.
How is the operation performed?
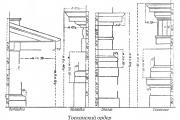
Surgery begins with providing access to the affected area. An incision 15–20 cm long is made along the joint, and the underlying tissue is pulled apart. Using special instruments, destroyed parts of bone and cartilage are removed. Articular surfaces before installing the implant, they are cleaned.
At the second stage, the prosthesis is installed. He can be:
- metal;
- silicone;
- ceramic.

The implant consists of a head, cup, stem and spacer. IN upper section a metal rod is screwed into the femur. After this, the head and liner are installed, giving the prosthesis mobility.
The surgeon adjusts the parts and checks the length of the leg and range of motion. The friction unit is determined and the implant material is selected. After checking, the prosthesis is fixed with medical cement. During one operation, hip and knee replacements can be performed. The operation is completed with antiseptic treatment of the wound and layer-by-layer stitching of tissue. The skin is tightened with metal staples.

Endoprosthesis replacement is performed under general anesthesia. The patient is in a state of sleep and does not feel pain. The anesthesiologist must take into account the state of the body of each person. Epidural anesthesia is sometimes used.
The average cost of the operation is 200 thousand rubles.
Possible complications
Every surgical procedure carries certain risks. develop in 1–2% of cases. The most common are:
- addition of bacterial infections;
- bleeding;
- bone damage;
- thrombosis;
- dysfunction of the pelvic organs.
The most common dislocation of the hip joint occurs.
Infection of the prosthesis is considered an indication for repeated replacement joint

Rehabilitation period
After surgery, the patient is placed in the intensive care unit. After the anesthesia wears off, he is transferred to the ward. You can get out of bed 5-6 times after joint replacement. On day 2 the patient can walk using crutches. Painkillers and anti-inflammatory drugs are prescribed.
Allows you to speed up the recovery process. Its duration depends on the complexity of the operation and the general condition of the body. On early stages are performed aimed at strengthening the muscles of the thigh and lower leg. They restore blood circulation and prevent the formation of swelling and blood clots.

Inpatient treatment lasts 7 days, after discharge they continue to use crutches or a walker. The wound must be kept dry and clean. You should avoid taking a bath until the suture is completely healed.
For a year after the operation, the patient is under the supervision of an orthopedist. The doctor teaches balance and stability when walking. Contact medical institution necessary if the following symptoms appear:
- persistent swelling and pain;
- elevated temperature;
- wound suppuration;
- decreased sensitivity of the limb;
- hematuria.

After hip replacement, it is forbidden to bend the leg sharply or strongly. You cannot quickly move the limb to the left and right, this contributes. You need to be able to move your hip correctly.
Proper nutrition plays an important role. The diet should include foods rich in calcium and iron. These substances are required for tissue healing and muscle normalization. You need to eat as much as possible fresh vegetables and fruits, sesame seeds, meat and fish.
After hip replacement, stress and increased loads are eliminated.
A special pillow is placed under the affected area to reduce tension. Exercises aimed at restoring the functionality of the joint should be performed regularly.
Recovery motor function after hip replacement surgery is a long process that requires a lot of patience from the patient. But, nevertheless, when the right approach During the rehabilitation process, complete restoration of the functional capabilities of the joint can be guaranteed.
Duration rehabilitation period directly depends on the reason for endoprosthetics, as well as on the condition of the ligamentous-muscular system in the area of the affected hip joint. If prosthetics are performed due to traumatic destruction, then strong active muscles will require a much shorter period of recovery than muscles weakened by prolonged, sometimes many years of development of cocarthrosis.
Preoperative preparation
Preparing the patient for the upcoming rehabilitation begins several days before the operation. The purpose of such training is to teach a person to behave correctly in the postoperative period. The patient learns to walk with the help of crutches or a special walker, and learns to perform some exercises that will be required to restore the function of the prosthetic leg. In addition, the patient gets used to the idea that this is the beginning of a long stage in his life - the stage postoperative rehabilitation.
Before surgery, the patient is examined not only by an orthopedic surgeon, but also by specialists from related specialties in order to determine the patient’s condition in more detail and develop the best plan for surgery and postoperative rehabilitation. The anesthesiologist selects the most suitable type of anesthesia.
First stage of rehabilitation
The operation lasts on average about two hours. Before completion, drainage is installed in the operated cavity and the wound is sutured. Drainage is needed to remove the postoperative hematoma; it is usually removed 3-4 days after surgery. The first day the patient is in the intensive care ward, where his condition and restoration of hemostasis are monitored. On the second day, if the dynamics are positive, the patient is transferred to the general ward.
Rehabilitation after hip replacement should begin immediately after surgery, in the first hours after the patient recovers from anesthesia. The first exercises consist of flexion and extension of the foot of the operated leg, rotation of the ankle joint, tension and relaxation of the anterior surface of the thigh and gluteal muscles. Such exercises improve blood flow and tone the muscles.

The first day the patient should not get out of bed. On the second day, with the help of a doctor - a specialist in physical therapy (physical therapy), the patient is allowed to rise and stand on his feet. Usually, patients are immediately allowed to step on the operated leg with the full weight of their body, but in some cases the attending physician may limit the load on the new joint. All movements of the patient in the postoperative period should be slow and smooth.
You need to get out of bed on the side of your healthy leg, gradually lowering it down from the bed and pulling the operated leg towards it. In this case, it is necessary to ensure that the hips do not diverge too much to the sides, and the foot of the operated leg does not turn outward. You can sit only by following the “right angle” rule: the bend of the leg at the hip joint should not exceed 90º. In other words, the bent knee should not rise above the endoprosthesis. You cannot squat down, you cannot cross your legs. When sleeping, it is better to use two pillows placed between your legs. You should not lean toward your feet while sitting on the bed, for example, trying to reach the blanket lying at your feet. You should also not bend over to pick up your shoes while sitting on a chair. At first, it is better to put on your shoes with outside help, or wear shoes without backs. Compliance with these rules is intended to prevent dislocation of the prosthetic joint.
It is important to remember that the new joint is still “free floating”; it is installed, but not fixed in the correct physiological position. To fix it, rehabilitation of the muscles and fascia cut during surgery and stitched back together is necessary. The fusion of dissected tissues occurs in approximately 3-4 weeks. During this period, you should not strain your hip muscles, especially while sitting or lying down. To ease the muscle load, it is necessary to move the operated leg slightly to the side.
The patient should already be prepared, and, first of all, morally, for the pain that he will have to experience in the early stages after the operation. But, overcoming this pain, the patient must learn to walk independently with the help of crutches or a walker. Also, when taking the first steps, the patient may feel dizzy, but, nevertheless, the person should not stop and continue walking with the support of medical staff.
For the first 4 days, the patient needs the most careful and strict care. This is the period when postoperative complications may occur. Infectious inflammations are especially dangerous; they are difficult to treat, sometimes even requiring removal of the endoprosthesis. Therefore, during the operation and during the period post-operative care The strictest aseptic and antiseptic measures are observed. Sutures are usually removed 10 days after surgery. After removal of the sutures, the patient is allowed to shower without covering the scar, provided that he does not rub it with a washcloth or towel.
Second stage of rehabilitation
The second stage begins on the 5th day after surgery. The threat of complications has already receded and the patient begins to feel the operated leg. Muscle weakness goes away, he steps on his foot more and more confidently when walking with crutches.
On day 5-6, you can begin to master walking up the stairs. When lifting, you need to take a step up with your healthy leg, then with your operated leg, and only then move the crutch up. When descending, everything should happen in the reverse order - first you should move the crutch one step lower, then the operated leg, and finally the healthy one.
The load on the new joint and muscle system should increase gradually. By increasing the number of movements, the muscle strength of the thigh muscles will also increase. It is important to remember that until the ligamentous-muscular corset around the endoprosthesis is completely restored, it must be protected from dislocation, observing the right angle rule.
You need to do the whole complex every day physical therapy exercises, do small walks of 100-150 meters several times a day. IN this period You should not rush things too much and put too much stress on the operated leg, although the patient is given a deceptive impression of recovery. Muscles and fascia that are not fused well enough can become injured, causing severe pain, and even dislocation of the implant is also possible.
Unfortunately, Russian realities are such that the patient remains in the hospital after surgery for only 10-12 days. Due to organizational reasons, long-term rehabilitation under the supervision of an orthopedic specialist is impossible in our country. Therefore, after the stitches are removed and in the absence of complications, the patient is discharged from the hospital. And from this moment on, it is he who bears all the responsibility for fulfilling the requirements of the rehabilitation program. And if a person shows laziness or weak character during this period, then the process of his rehabilitation may drag on indefinitely.
Third stage of rehabilitation
 4-5 weeks after endoprosthetics, the muscles are already strengthened so much that they become able to withstand more intense loads.
4-5 weeks after endoprosthetics, the muscles are already strengthened so much that they become able to withstand more intense loads.
It's time to move from a crutch to a cane. To do this, it is necessary to restore the coordinated work of all thigh muscles, and not just those that directly surround the endoprosthesis. Until now, the patient was instructed to make all movements smoothly and slowly, but now he will have to learn to balance and react to sudden shocks and movements.
At this stage, exercises with an elastic band, which must be pulled back and forth with the operated leg, as well as exercises on special simulators, are very useful. Training on an exercise bike with short or long pedals is allowed, provided that the right angle rule is observed. First you need to learn how to pedal backwards, and only then forward.
Balance training involves maintaining balance while standing on both the healthy and the operated leg. To begin with, you can hold on to the handrails or the wall, changing your legs. Then you can add leg swings with an elastic band attached to it. Such exercises will help the patient strengthen the entire set of thigh muscles as a whole.
The step, a small elevated platform for doing step aerobics, is also very good for balance training. At a low step, the patient can take steps up and down, forcing the muscles to work. Such exercises are very good for training balance.
The exercise therapy complex also includes treadmill. To strengthen the ability to balance on it, you need to move not towards the movement, but, on the contrary, in the direction of movement. In this case, the foot should roll from toe to heel, and the leg should fully straighten at the moment when the foot rests completely on the surface of the track.
And a mandatory requirement for hip joint rehabilitation is walking. At the very beginning of this stage, walking time should be no more than 10 minutes. You should gradually increase the duration of walks, bringing their time to 30-40 minutes, doing them 2-3 times a day. As your sense of balance strengthens, you should gradually abandon the cane in favor of walking without support. After complete recovery, it will be extremely useful for the patient to maintain the habit of walking for 30-40 minutes, 3-4 times a week. This will allow him to maintain tonus of the ligamentous-muscular apparatus, promoting general strengthening body.
You can conduct the following test to assess the quality of timed rehabilitation: at a signal, get up from a chair and walk 3 meters forward and backward. If the following indicators are achieved, then you can increase the intensity of the load:
- patients aged 40-49 years – 6.2 seconds;
- patients aged 50-59 years – 6.4 seconds;
- patients aged 60-69 years – 7.2 seconds;
- patients aged 70-79 years – 8.5 seconds.
The forward bend test can also be used to evaluate rehabilitation. The essence of this method is that the end of a centimeter tape is fixed horizontally on the wall at the level of the patient’s shoulder. The patient stands sideways to the wall and leans forward while standing still. To move to the next stage the following indicators must be achieved:
- men under 70 years old – 38 cm;
- men over 70 years old – 33 cm;
- women under 50 years old – 40 cm;
- women 50-59 years old – 38 cm;
- women 60-69 years old – 37 cm;
- women over 70 years old – 34 cm.
Fourth stage of rehabilitation
This stage begins approximately 9-10 weeks after surgery. By this time, the patient’s muscles and sense of balance had already noticeably strengthened, and he had learned to walk without a cane. But this is not the end of rehabilitation and in no case should we stop there. The process of restoring the motor function of the operated hip joint must be completed. If you stop at this stage, then the pain in the endoprosthesis area may resume. But many patients during this period are lazy to continue training and are ready to endure minor pain, since it is much weaker than the pain they experienced before surgery, as well as postoperative pain.
You should continue exercising on the exercise bike and treadmill in forward and backward directions.
You can train the hip abductors by stretching an elastic band with your knees, as well as the adductors by squeezing a pillow between your legs. To strengthen the gluteal muscles, they should be squeezed and unclenched. You need to master walking backwards, including on stairs, and use a higher step to train your balance. Balancing on two legs without support on a bus or tram also strengthens your sense of balance. We must strive to improve the standards of the forward bend and timed walk tests.
If the patient takes the fourth period of rehabilitation seriously, then he can be sure that the endoprosthesis that replaced his own hip joint will never fail him in a critical situation when a quick muscle reaction is required: for example, if he slips on ice, stumbles, or gets into Road accident. Maintenance muscle tone necessary even for completely healthy people, and for people who have undergone hip replacement surgery, this is doubly important.
moisustavy.ru
How does healing occur?
The hip joint is the largest joint in the entire body: it needs to support all the weight and, in addition, perform about 40% of all movements that a person makes. This is mainly the movement of the hip back and forth and to the sides, as well as its rotation. This joint is also involved in the rotation of the entire body.
All movements are possible thanks to a large number of muscles. They fan out from the hip joint, attaching to its structures. Nerves and blood vessels pass between the muscles. And so that the femur does not “jump out” of the acetabulum, it is secured by the same “fan” of ligaments. Between individual ligaments and muscles there are formations that resemble small joint capsules. They are needed to reduce friction of structures when performing movements.
 When a joint “becomes unusable” and needs to be replaced, that is, prosthetics, surgeons do the following. In order to get to the joint, 2 large muscles (medium and gluteus maximus), attached to the femur, are released from the fascia. They are moved aside and separated with a blunt instrument, that is, the muscle bundles, although not cut, are separated. Then one mucous bursa is dissected and an incision is made in the gluteus minimus muscle, and then in the articular bursa. The femur is cut at the level of its neck, after which it is removed from the soft tissues of the thigh. An artificial joint is placed and fixed in place of the removed bone. All muscle incisions are sutured.
When a joint “becomes unusable” and needs to be replaced, that is, prosthetics, surgeons do the following. In order to get to the joint, 2 large muscles (medium and gluteus maximus), attached to the femur, are released from the fascia. They are moved aside and separated with a blunt instrument, that is, the muscle bundles, although not cut, are separated. Then one mucous bursa is dissected and an incision is made in the gluteus minimus muscle, and then in the articular bursa. The femur is cut at the level of its neck, after which it is removed from the soft tissues of the thigh. An artificial joint is placed and fixed in place of the removed bone. All muscle incisions are sutured.
To ensure normal function of the new joint, it is necessary for the muscles that were cut and separated to heal well and correctly. They will do this if:
- The sheath of the muscle fibers will not be damaged: directly below it lie satellite cells (companions), which turn into new muscle cells. If the shell is damaged, instead muscle fiber a scar forms;
- normal blood supply to the cut or pulled apart fibers will be restored;
- new branches of nerves will appear in this area;
- damaged muscles will be constantly under tension.
These conditions will be met if:
- the load will be temporarily taken over by those muscles of the same thigh that were not damaged;
- The muscles of the foot and lower leg will work, improving blood circulation in this leg.
What you need for a successful recovery
In order for rehabilitation after hip replacement to be successful, you must follow these rules:
- forget about laziness if you want your relative to recover in less than a year, and not stretch this process out for an indefinite period of time, simultaneously “earning” depression;
- Rehabilitation measures should be started immediately after the restoration of adequate consciousness on the first postoperative day. The first steps are absolutely simple;
- a set of measures is important: it is not that today only breathing exercises are performed, and tomorrow - exercises for the muscles of the operated leg, and every day - a variety of actions;
- the actions performed must be consistent: on the first day after the operation you can perform one type of load, then another, but there should be no “jumps”;
- rehabilitation measures must be carried out continuously. Long breaks are unacceptable.
What are the consequences of lack of proper rehabilitation?
 If rehabilitation after endoprosthetics is not carried out at all or is carried out without the necessary sequence, the injured muscles lose their tone, and scars may form at the incision sites. If the limb is not strained, the ligaments will also heal in a stretched position. This will lead to:
If rehabilitation after endoprosthetics is not carried out at all or is carried out without the necessary sequence, the injured muscles lose their tone, and scars may form at the incision sites. If the limb is not strained, the ligaments will also heal in a stretched position. This will lead to:
- dislocation of the head of the prosthesis;
- bone fracture near the prosthesis;
- inflammation of one or more nerves located near the prosthesis.
Planning of rehabilitation measures
The rehabilitation period after endoprosthetics lasts about a year. Conventionally, it is divided into 3 periods:
Early period: from the first day after surgery to 3 postoperative weeks. It is conventionally divided into 2 motor modes:
- Gentle: 1-7 days of the postoperative period. At this time, inflammation of the wound caused by the operation occurs;
- Toning: 7-15 days. At this time, the postoperative wound heals.
Both of them are fully supervised by a doctor rehabilitation medicine.
Late period. It is carried out first in the physical therapy room of a polyclinic at the place of residence, where a person should go immediately after discharge from the hospital. Then the set of exercises continues to be performed at home. It is optimal if the relatives of the operated patient help to develop the joint, encourage him and prevent him from missing classes.
It is divided into 2 motor modes: 1) early recovery: 15-60 days, when “utilization” of bone structures occurs; 2) late recovery: from 45-60 to 90 days, when the internal structure of the femur is restored.
Remote period: 3-6 months when the femur takes its final shape and structure. It is advisable to carry it out in specialized sanatoriums or hospitals.
The individual training program is drawn up either by a rehabilitation doctor or by a physical therapy doctor at the hospital where the operation was performed. Before developing a set of exercises, they must familiarize themselves with the medical history, which describes the nuances of the operation, talk with the patient, find out about his state of health and previous diseases. Also, the rehabilitation medicine doctor should look at the range of motion in the operated limb and exercise tolerance.
Preoperative rehabilitation
 If a lot of time has passed from the onset of the hip joint disease to the completion of its prosthetics, then rehabilitation should begin even before the operation. This is explained by the fact that due to long-term pain, a person spares his leg, as a result, the muscles of this limb become hypotrophied, which leads to:
If a lot of time has passed from the onset of the hip joint disease to the completion of its prosthetics, then rehabilitation should begin even before the operation. This is explained by the fact that due to long-term pain, a person spares his leg, as a result, the muscles of this limb become hypotrophied, which leads to:
- limited mobility in the hip joint;
- pelvic tilt to one side;
- walking disorder;
- reducing the severity of the forward convexity of the spine;
- the appearance of scoliosis.
Therefore, in the preoperative period, such people who have been suffering from coxarthrosis for a long time, mainly elderly and senile people, need to be prepared. For this:
- provide training in the use of crutches to form a correct gait without relying on the sore leg;
- perform electromyostimulation of both gluteal areas and thighs on both sides. It involves applying electrodes of a special apparatus to the motor zones of the desired muscles, after which, under the influence of current, they contract;
- perform exercises: flexion and extension of the foot, getting out of bed so that excessive flexion in the hip joint does not occur;
- teach deep and diaphragmatic breathing;
- carry out therapy that improves the condition of the cardiovascular system.
Rehabilitation in a hospital - an early stage of rehabilitation measures
This stage, although it takes place entirely in the hospital, always raises many questions. And doctors, who are constantly busy, do not always answer them completely and intelligibly. Therefore, we will look at each step in detail.
Period goals
At this stage you need:
- create conditions for the formation of new vessels that will nourish the joint;
- provide conditions for healing of the suture;
- avoid complications: thrombosis, stroke, congestive pneumonia, bedsores, wound suppuration;
- learn to get up, sit up in bed, and walk correctly.
What to do on the first day?
 Rehabilitation after hip replacement begins from the first minutes after a person wakes up from anesthesia. It consists in:
Rehabilitation after hip replacement begins from the first minutes after a person wakes up from anesthesia. It consists in:
- moving the toes of the affected leg: every 10 minutes;
- flexion and extension of the toes of the operated leg: 6 approaches per hour;
- pressing both heels on the bed for 6 times. Toes point up, feet parallel to each other;
- movement of the arms: rotation of the hands, bending of the elbows, raising of the shoulders, swinging the arms;
- tension (without bending or other movement) of the buttocks, thighs and lower legs - but only on the healthy side. This is called isometric tension.
After 2-3 hours, the ankle joint of the operated leg should be involved in movement: here light flexion-extension, rotation of the foot clockwise and counterclockwise are performed.
Monitor the urination of the operated relative: he should urinate in the next 1-2 hours after the operation. If he cannot do this even with the water tap on (not yet in the toilet, but on a duck or a vessel), be sure to tell the medical staff on duty. The patient will be given a urinary catheter and urine will be drained.
Breathing exercises
First breathing exercise performed as early as possible in a lying position. The patient lies with his arms either along the body or placed to the sides. A deep breath is taken - the stomach is “like a ball.” Exhale - the stomach relaxes.
When the patient is allowed to sit (how to sit - see section “16 important rules early period"), breathing exercises expand. To do this, you need either balloons, which a person will inflate once every 3 hours. On the first day, you can “make do” with a tube lowered into a glass of water: you will need to blow air through it.
Vibration massage
In a sitting position, with the patient's head tilted, perform vibration massage of the chest. To do this, apply camphor oil to the skin of the chest from the back and rub your back in a circular motion. Then place the palm of one hand on your back, on the side of the spine, and with the fist of the other hand, perform light blows on your palm. You need to “work” the chest from bottom to top.
Psychological moments
 Loving relatives should not wait until their elderly, operated parent expresses a desire to begin performing simple exercises - they need to do it themselves, with his limbs. Elderly people often lie in apathy for a long time after stress, one of which is surgery, and may even fall into depressive state. In the process of exercising with them, when a stream of impulses arrives from the working muscles to the brain, endorphins are produced, and this mood will pass.
Loving relatives should not wait until their elderly, operated parent expresses a desire to begin performing simple exercises - they need to do it themselves, with his limbs. Elderly people often lie in apathy for a long time after stress, one of which is surgery, and may even fall into depressive state. In the process of exercising with them, when a stream of impulses arrives from the working muscles to the brain, endorphins are produced, and this mood will pass.
Anesthesia
The surgeon who performed the operation, in his prescription sheet, which he writes to the nurses, indicates the prescribed drugs (antibiotics, blood-thinning drugs) and the frequency of their administration. As for painkillers, it is prescribed: on demand, but not more than such and such an amount per day. Therefore, the nurse will ask the patient whether to administer the drug or not. And when the pain intensifies, you should not endure it, but call it for your elderly relative.
Prevention of thrombosis
 This is a very important aspect, and here's why. Vienna lower limbs have great extensibility: if a person lowers his legs below the level of the heart, almost ½ of all available blood remains in these veins. In order to reach the heart, this blood must rise against gravity, so it does this slowly, and the leg muscles “pump” it upward.
This is a very important aspect, and here's why. Vienna lower limbs have great extensibility: if a person lowers his legs below the level of the heart, almost ½ of all available blood remains in these veins. In order to reach the heart, this blood must rise against gravity, so it does this slowly, and the leg muscles “pump” it upward.
If a person moves little and sits almost all the time, all the conditions are created in the veins of the legs for the formation of blood clots there. The risk of blood clots increases with varicose veins when “sacs” appear in the veins, convenient for blood clots to settle. These blood clots can “fly off” and enter the arteries of the lungs or brain along with the bloodstream, but this is partially prevented by the muscles of the lower leg, which have a certain tone even during rest and sleep.
Fortunately, it can be reduced. For this:
- Before the operation, you need to buy elastic bandages, which are given to the operating room with the patient. When the surgeon completes the operation, his assistants bandage both legs: this creates a semblance of that muscle tone that is always present in the lower leg muscles.
- Before sitting up in bed or standing up after surgery, you need to make sure that your relative's legs are well bandaged.
- When preparing for surgery, you must take a blood test for coagulation (coagulogram), and if the results are higher than normal, you must undergo a course of treatment. For this purpose, antiplatelet agents (Aspirin and the like) may be prescribed, as well as local treatment(treatment of feet with heparin gel or Lyoton). There is no need to undergo surgery until the INR reaches 0.9-1 units.
- In the postoperative period, it is necessary to administer blood-thinning drugs (Clexan, Enoxyparin and others) for at least 10 days, and better yet, up to 14 days under the control of a coagulogram and clotting time (this test is taken from a finger prick).
Diet
In the first days, when postoperative intestinal atony is possible, the diet should contain only liquid and semi-liquid, easily digestible foods. These are vegetable soups with ground vegetables and meat, second broths, slimy porridges with ground in a blender chicken meat or lean beef.
Further, the diet is expanded, but in order to avoid exacerbation of diseases digestive tract, this should not include smoked meats, fried dishes and those containing marinades and hot sauces. Overeating sweets with such a sedentary lifestyle is also not recommended - fermentation processes in the intestines will intensify.
When can you sit and stand up?

The doctor should say this based on the specific situation. In some cases, this can be done after 6-8 hours, but usually only the next day.
16 Important Early Rules
- For the first 5 days, sleep only on your back.
- At the end of the first day, you can turn on your side, but only with the help of a health care worker and only on your healthy side.
- Lying on your side, place a small pillow between your legs to keep your gluteal muscles toned at all times. Do not bend the affected leg more than 90°: the knee of this leg is below waist level - not level and not higher.
- When lying on your back, do not place your legs on top of each other or very close: a small wedge-shaped pillow should be placed between them.
- When lying on your back, place a small cushion under your knee: this will help relieve pain. Place another roller or rolled towel on the outside of the operated thigh - it will prevent the leg from hyperextending. These rollers need to be removed periodically. It will be possible to completely get rid of them only after 1-1.5 months.
- To understand whether your foot is lying correctly, use the big toe test. To do this, place your thumb on the operated leg, closer to its outer surface. If the knee is on the outside of the big toe (that is, the right knee is even more to the right or the left is even more to the left), then everything is correct and the leg muscles are not overstrained.
- You will be able to turn onto your stomach after 5-8 days.
- There should be no sharp turns or rotations in the hip joint.
- It will be impossible to squat for a long time.
- Before lying on your back or sitting down, you need to spread your legs slightly to the sides.
- You can only sit on chairs of a design that will not allow your knees to be higher than the level of your navel, but will ensure a right angle between the seat and the hip joint.
- Hospital shoes must be flat.
- When changing into street shoes, the operated person needs help. If this is not possible, he should do it himself only with the help of a spoon.
- You will need to sit up in bed using your hands.
- If you need to get something from the foot end of the bed (for example, a blanket), it is better to ask for help, since you can sit down, but you cannot bend down below the level of the navel. If there is no one to help, you will have to take what you want by getting out of bed.
- Walk - only without relying on the operated limb.
What to do on the second day after surgery?
Breathing exercises, vibration massage and drug treatment are carried out to the same extent. It is on this day that most operated people are allowed to stand up for the first time. How to do this - read the section below.
The following are added to the exercises described above:
| Initial position |
Description of the exercise |
| Lying on your back, cushion between your knees |
Bend both legs at the knee joints at an angle of at least 90 degrees, rest your feet on the bed. Next, sliding movements are performed on the bed: in one direction - pause - in the other - pause. |
| Same |
Raise your hands up, bend them into fists, stretch your hands behind your head while take a deep breath. As you exhale, lower your arms and unclench your fists |
| Same |
Raise one leg up at an angle of 10-15 degrees. As you inhale, raise your head and look at your foot. As you exhale, relax. Repeat the same with the other leg. |
| Same |
Using sliding movements, as in the first exercise, imitate walking with your feet |
| Same |
Having bent your leg at the knee joint, tilt it in outside, fix it, return it to its previous position, and then, with a sliding movement, lay it on the bed. Repeat with the other leg. |
| Same |
As you inhale, raise your arms to the sides behind your head and stretch; as you exhale, lift yourself up and reach for your feet with your hands, looking at your fingertips |
After the operated person has stood confidently, without dizziness, there is no need to immediately go far. It is better to prepare for walking with exercises. To do this, you need to turn around to face the headboard, leave the crutches and hold on to the headboard. Now, standing on your healthy leg, perform the following exercises:
- Abduction and adduction of the operated leg to the healthy one. To do this, you need to bend it slightly at the knee.
- Gently move the affected leg back and forth. This exercise should not cause pain.
After this, you need to sit, swing your arms and breathing exercises, and then lie down and relax. It is better to postpone getting up again for 1-2 hours. You will have to go to the toilet on a boat or a duck.
From the second day, physiotherapy is usually prescribed in the amount of 3-5 procedures: UHF, magnetic therapy, diadynamic currents. This is very important: the procedures will help quickly eliminate swelling and pain in the limb. Physiotherapeutic procedures are carried out in the ward using a portable device.
How to get up?
You need to follow the algorithm:
- Check if you have an elastic bandage, compression stockings or tights if prescribed by your doctor. The patient should not wear such underwear himself: there is a risk of hyperextension of the operated joint.
- Call the nurse.
- Together with the nurse (she will help a little and control the extension of the leg), helping yourself with your hands, you need to sit down with your legs hanging off the bed:
a) Using your hands, you first need to hang the operated leg from the bed;
b) Dangle your healthy leg;
c) Take a crutch in the hand on the side of the operation performed;
d) Place the other hand (opposite to the operated side) on the health worker’s shoulder;
e) Stand up, leaning more on the crutch, less on the nurse, and under no circumstances standing on the sore leg.
- You can sit in bed for a while, but to do this you need to put several pillows under your back.
- Make sure that the hip joint is always higher than the knee.
- If you don't feel dizzy, you can try standing up. This requires the help of a nurse, as well as crutches or a walker.
How to walk?
The healthy leg is positioned slightly behind the crutch line or slightly in front of it. Now a step is taken with crutches, and the operated leg comes out to the line of the crutches and is placed on the floor, but the body weight is not transferred to it. The body is straight, the foot does not turn outward.
After this, the healthy leg takes an extension step. Then the movements are repeated: step with crutches - step with the healthy leg. For the first time, this is monitored by a physical therapy instructor, who comes up to the ward specifically for this purpose.
Third to seventh day
During this period, breathing exercises and vibration massage continue to be performed. Drug treatment– the same and the diet is the same. But the need for painkillers is already beginning to decline.
You can already sit up in bed without outside help, but only with the help of hands and support (over-bed frame or “reins”). It is recommended to walk first for 10, then 15 minutes twice a day, only while supporting yourself on a crutch.
New exercises and physical procedures are being introduced.
Isometric tension
From 3-5 days, they gradually begin to perform isometric tension exercises: they strain the foot on the operated side for 1-1.5 seconds, then relax it; strain the lower leg for 1-1.5 seconds - relax the leg, then do the same manipulation with the sore thigh and buttock. All joints of the leg are motionless. After this, the same exercise (but only with a longer duration of tension) is performed on the healthy side.
Isometric tension exercises are performed 3 times a day. Gradually, the time of muscle tension in the affected leg is increased to 3 seconds, then to 5 seconds.
Electromyostimulation
Elderly and long-term ill people begin to undergo the electromyostimulation procedure on a healthy leg from the 3rd day. It is performed 3-5 times a day, for 15 minutes, and should improve the preparation of the leg for the increased load on it.
On the operated limb, this manipulation is performed only after the sutures are removed: in a clinic or, by agreement, at home.
Changes in body position
From 5-8 days you should try to lie on your stomach so that you get 5-10 turns per day. The legs in this position should be slightly apart at the hips. To do this, place a small pillow between them.
Healthy leg massage
Manual treatment of the soft tissues of the non-operated limb helps improve blood circulation and muscle function. This way the healthy leg will get less tired due to the increased load on it.
Massage is indicated for everyone who has undergone surgery, but first of all it should be performed by those whose second hip joint has also undergone degenerative processes. Otherwise, there is a high risk of undergoing endoprosthetics of a second joint while still recovering from one operation.
Exercises
| Initial position |
Exercise |
| Lying on your back, legs straight, a cushion between them |
Extend and lower your legs for 5-6 approaches. |
| Same |
Imitate walking with your feet for 10 minutes. You need to repeat this exercise 5-10 times a day. |
| Same |
The operated leg is straight and lies relaxed. Bend your healthy leg at the knee, lean on its foot and try to raise your pelvis as high as possible, holding it in this position for 5 seconds. Slowly lower your pelvis. You need to perform 5-10 approaches 5-8 times a day. |
| Same |
Raise your straight legs one at a time |
| Same |
Gradually, using your hands, lift your torso |
| Same |
Bend one leg slightly at the knee and press that heel into the bed. Place your foot in a sliding motion. Do the same as with the other leg. |
| Sitting on the bed, legs dangling. The back is straight |
Straighten your knees and hold your shins in this position for about 5 seconds. You should gradually try to reach 10-20 approaches, repeating 5-6 times a day. This is possible if there is no deterioration in the heart and respiratory systems. |
| As in the previous exercise |
As you exhale, make a movement as if you are pushing your torso up |
| As in the previous exercise |
Bend your knees |

Tonic period
It begins on the 7th day and is ideally carried out in a special rehabilitation department, under the supervision of a rehabilitation physician and exercise therapy instructor.
During this period, the motor mode expands: a person can already train to walk 3-4 times a day. As soon as he can move at a calm pace more than three times a day for 15 minutes, rehabilitation program exercises on an exercise bike are included. They are carried out for 10 minutes once a day, then for 10 minutes twice, starting at a speed of 8-10 km/h with a gradual addition of power load. Cycling exercises are performed under the control of pulse and blood pressure.
The exercises are performed the same as in the previous period, only the number of their approaches increases.
During the same period, they are taught to walk up stairs.
How to walk up the stairs
- Grab the railing with your unaffected side.
- When going up, the healthy leg steps first, then the sore leg, then the crutch (at this stage these are both crutches folded together).
- During the descent: the crutch walks, then the operated leg, then the healthy leg.
When are the stitches removed?
This is done for 12-14 days. 1-2 days after removing the stitches, you can take a full shower.
When discharged
If the postoperative period is uncomplicated, discharge is carried out on days 14-21. If the patient is severely weakened or in this hospital This is how it is accepted, he can be transferred to the rehabilitation department for another 1-2 weeks.
Preparing the home before the arrival of an operated relative
To prevent injury to the operated leg, before discharging an elderly relative home, you need to prepare the apartment (house):
| Bed |
It is advisable to purchase a functional bed in which you can raise the headrest and also change the height (using a lever). Standard models of such beds are equipped with wheels, therefore, when buying a used model, it is important to check that the brake works well, otherwise the operated relative risks falling. It is optimal if the bed is equipped with an over-bed frame with a hanging triangle, which you can grab and sit on |
| Floors |
Before arriving, remove any carpet runners that could be caught on by a crutch. If the floor is cold, it is better to lay a carpet that will be “stretched” so that it cannot get caught |
| Toilet |
One seat is not enough to ensure an angle of less than 90 degrees between the hip and torso. Therefore, you need to purchase an additional semi-rigid pad |
| Handrails |
They need to be driven into the walls: on the wall near the bathtub, on both sides of the toilet, in the corridor where a person puts on his shoes (he cannot sit on a low chair for a year) |
| Bathroom |
A person will have to wash while sitting throughout the year, so the shower or bathtub should have either a chair with non-slip legs or a board attached so as to ensure a hip flexion angle of less than 90 degrees |
| Chairs |
They must be rigid or semi-rigid, of sufficient height |
| Railings along the stairs |
If they were not there, they will need to be installed |
Late recovery stage
The late period of rehabilitation after hip replacement begins on the 15th postoperative day.
From the very beginning of the period, a massage of the sore leg is included: the soft tissues of the operated hip are worked out with careful, non-traumatic movements that should not cause pain.
Prohibitions during this period:
- You still cannot bend your leg so that the angle between the thigh and the body is less than 90°.
- The operated leg should not be turned inward (so that the big toe is pointing towards the opposite heel) and placed (and placed) close to the healthy leg.
- sleep on healthy side- prohibited.
- You should not put your body weight on your sore leg.
- Sitting on a low chair is contraindicated.
- Exercises that are accompanied by pain are prohibited. When exercising and walking, it is only permissible light feeling discomfort, which goes away after a 2-3 minute rest.
- Long-term (more than 40 minutes) sitting, as well as sitting with crossed legs, are contraindicated.
- Relatives should help you put on compression garments or elastic bandages. Otherwise, the artificial joint, which has already begun to fix itself, may dislocate, which will result in a new operation.
- Walking without support is contraindicated.
It is already possible to wash the dishes yourself and prepare “quick” meals while leaning on a crutch.
More complex ones are added to the exercises from the previous period:
- I.p. lying on your back. With your knees bent, perform movements that imitate riding a bicycle.
- I.p. on the back. Bend your leg at the knee, pull it towards your stomach, and fix it with your hands for 5 seconds. Repeat with the other leg.
- I.p. lying on your stomach. Bend and straighten your knees to avoid pain.
- I.p. on the stomach. Raise your straight legs one at a time.
- I.p.: facing the headboard of the bed, holding it with your hands. Slowly lift one leg or the other.
- I.p. Same. Standing on one leg, move your other leg to the side. Repeat the same with the other leg.
- I.p. Same. Bend your knees one by one and take them back in this position. The hip joint should extend slightly.
A month after walking confidently with a crutch, you can try replacing the crutch with a cane.
Long-term rehabilitation period
It starts 90 days after surgery. After 4-6 months it will be possible to walk without a crutch or cane (the doctor will tell you the exact figure). Breathing exercises are no longer carried out during this period, but exercise therapy and physiotherapy are integral components of recovery.
- pearl or oxygen baths;
- applications of paraffin or ozokerite to the area of the operated joint;
- underwater shower-massage;
- laser therapy;
- balneotherapy.
Add new ones to the previous exercises:
| Initial position |
Performance |
| Lying on your back |
Cross your legs and turn them at a slight angle in one direction, then in the other direction. |
| Same |
Do “scissors” with straight legs, either bringing your legs together or spreading them apart |
| Same |
With the toe of one straight leg, touch the area on the outside of the other leg (your thighs will lie on top of each other) |
| Same |
Raise one straight leg to the maximum possible position - lower it. Do the same with the other leg. |
| Same |
Bend one leg at the knee and slide it up, then down. Repeat with the other leg |
| Same |
Bend one leg at the knee, pull it towards your chest and hold it with your hands. Repeat with the other leg |
| Same |
You need to bend the knee joint and pull two legs towards your chest, but without using your hands |
| Sitting on a gymnastic mat, with your hands supported behind your back |
Raise your knees bent |
| Sitting on a chair |
As you slide one foot over the other, pull your knee toward your chest. Repeat the same with the other leg |
| Standing near a chair |
Place your healthy leg, bent at the knee, on a chair. Now lean towards that knee joint |
| Standing near a chair |
Hold the back of a chair and do squats |
| Standing without support |
Do squats |
| Standing sideways near the headboard |
Carefully, holding onto the bed, squat, but so that the angle between the thigh and body is less than straight |
| Standing near a step platform (a stable wide block) 100 mm high |
Step onto and off the step platform with your good foot first. Tempo: slow, repeat 10 times |
| Standing near the headboard, with an elastic band on the operated leg, above the ankle joint. The tourniquet is attached to the bed leg |
Bend your leg, fixed with a tourniquet, at the knee and stretch it forward. Then turn sideways so that you can swing your leg to the side. Slow pace, repeat 10 times |

nasledie.center
Hip replacement rehabilitation
Depending on the reason that led to the need to replace the hip joint, the timing of the start of certain exercises may vary. The more active the patient was before surgery, the earlier active activities should begin. For patients who are deprived of full range of motion before endoprosthetics (for example, with severe arthrosis), it may take more time to develop and bring atrophied muscles to normal tone.
General principles of exercise in the early period after surgery (up to 6 weeks) can be identified:
- Starting from the first postoperative day, it is necessary in bed (and then sitting with support on the back of a chair) to perform light, slow movements in the ankle joint - raising and lowering the foot; rotating the foot clockwise and back;
- Work the muscles of the thigh and buttocks (gradually bending the leg at the knee with the heel resting on the bed; lifting or abducting the straightened leg);
- During classes, it is forbidden to rotate (rotate) the leg inward;
- Crossing your legs, squats, and excessive flexion at the hip joint, bringing the leg to the body more than 90 degrees, can harm recovery.
- While sitting, check the correct position of your thighs relative to the floor (they should be parallel) and move your knee slightly outward;
- Going up and down the stairs must be carried out in a special order (move the healthy leg to the top step, pulling up the operated one; when going down, first move the leg with the endoprosthesis, and then the healthy one);
- You cannot sit with your legs crossed.
Advice!!! To avoid unconsciously changing the position of your legs during sleep, you can use a simple trick: place soft rectangular pillows between your legs.
How long will rehabilitation take?
After a certain time, many restrictions on movement can be removed, because... fusion of muscles and tendons damaged during surgery will occur. After hip replacement, rehabilitation takes place in a time frame that is individual for each patient. Current monitoring of the survival rate of the endoprosthesis is mandatory at 3, 6 and 12 months, and then annually. In any case, after 2 months there is a significant increase in the patient’s motor activity, and the list of permitted movements depends on the course of the postoperative period and the initial state of health.
artroclinic.ru
Rehabilitation periods after hip replacement
There are three periods of rehabilitation. They all deserve to be faithfully executed. necessary recommendations and close attention. Before taking any action, it is better to think carefully.
The main rule: do not harm yourself!
 Patients usually stay in hospital for about three weeks. This time is quite enough to teach a person how to lie, sit, walk, climb stairs, and walk on crutches correctly.
Patients usually stay in hospital for about three weeks. This time is quite enough to teach a person how to lie, sit, walk, climb stairs, and walk on crutches correctly.
- Early period– begins immediately after surgery and lasts about two weeks. Light gymnastic exercises should be done now.
- Late period– duration is 2 and a half months (from the 15th day after surgery to three months). The hospital stay ends and the patient ends up at home.
- Functional recovery period takes the longest period of time. On average, it lasts 3 months (from the third to the sixth months after the intervention).
Early period after hip replacement
Bed rest for the first day, but active. You can do some exercises, breathing exercises, and sit down. The legs are fixed in a special position, that is, a bolster is placed between them and the operated leg is moved to the side.

Correct lying position
On the second postoperative day, dressing is performed, then it is done once every 2-3 days. After about a couple of weeks, the stitches are removed.
In the first couple of days, a diet is prescribed that excludes foods that promote gas formation, salt, and sugar. It is allowed to eat porridge with water, jelly, and fermented milk products. Next, the doctor prescribes nutrition depending on the presence of certain concomitant diseases.
After a couple of days, you are allowed to sit on the edge of the bed. For the first time, everything is done under the supervision of medical personnel. This is especially true for the first time getting out of bed, if the doctor gives the go-ahead.
The purpose of the exercises: improve blood circulation and prevent the formation of blood clots, increase muscle tone.
Exercises for rehabilitation
- Moving the toe towards and away from you. Several times every 10 minutes.
- Rotation of the foot with change of direction.
- Tighten your knee and try to press your leg to the bed, as if straightening it. Stay in this position for 5-10 seconds.
- Tighten your butt muscles. Press your heels into the bed for 5-10 seconds.
- Bend your knee and drive your heels toward your hip joint. In this case, the angle should not be more than 90 degrees.
- All exercises are performed slowly, every hour on both legs, 5 approaches.
- When you tense your muscles, inhale and when you relax, exhale. Such gymnastics helps prevent the development of congestion in the lungs.
- You are only allowed to sleep on your back in the first days; you can only roll over onto your stomach after a week.
- The angle of flexion of the leg is no more than 90 degrees.
- Before you want to sit down, don't forget about elastic stockings or bandages. They are necessary to prevent the formation of blood clots.
During the early period of rehabilitation after hip replacement, the patient needs to learn to follow the doctor’s recommendations, do the permitted exercises, breathing exercises, and also sit up in bed, turn onto the stomach and healthy side.
Late period of rehabilitation
 It's time to learn how to get out of bed, stand in a stable position and walk. You will need to learn how to perform all these actions independently and, most importantly, safely. It is important to first hear theoretically about how to perform an action correctly and only then perform it correctly. Of course, under the supervision of medical professionals.
It's time to learn how to get out of bed, stand in a stable position and walk. You will need to learn how to perform all these actions independently and, most importantly, safely. It is important to first hear theoretically about how to perform an action correctly and only then perform it correctly. Of course, under the supervision of medical professionals.
Getting out of bed
All movements begin on the healthy side, the healthy leg.. It is necessary to sit on the edge of the bed, and the operated leg will be straightened and placed forward. Next, the feet are placed on the floor. The non-operated leg acts as a support, the crutches are placed in front, the leg is slightly bent and brought to the level of the crutches. Now lean on your crutches and stand up. To go to bed, do the same thing only in reverse order.
Walking
First with the help of crutches, then with a cane, you will learn to walk again. The doctor will tell you how to deal with the load on the operated leg. Either he will immediately allow you to stand on your leg with full weight, or he will limit the load on the replaced joint, gradually increasing it. It is important to walk little and far, not to overdo it.
Exercises
The list of exercises that you did in the first period of rehabilitation after endoprosthetics is supplemented with several more:
- Raise the operated straightened leg forward to a distance of about 30 centimeters. Put it back straight as well.
- The operated leg is moved to the side by 30 centimeters. Then back.
- The operated leg is retracted back and forth.
- Raise the knee of the operated leg up, the foot lifts off the floor by 30 centimeters. You need to hold your leg in this position for a few seconds.
All exercises are performed in a standing position with support on some object.(back of a chair or bed). 10 repetitions, about 10 sets per day. Make sure your toes and knees are facing forward. You can proceed to these exercises only if you have a stable standing position and confident walking.
Climbing and descending stairs
 An important step after endoprosthetics is teaching the patient how to go up and down stairs. This is also a kind of exercise. Not a single person can do without this skill. You can start training when you have mastered proper walking on crutches. It is best to hold on to the railing with the hand on the side of your healthy leg. 1 step - 1 step.
An important step after endoprosthetics is teaching the patient how to go up and down stairs. This is also a kind of exercise. Not a single person can do without this skill. You can start training when you have mastered proper walking on crutches. It is best to hold on to the railing with the hand on the side of your healthy leg. 1 step - 1 step.
The ascent begins with the healthy leg, the operated leg is placed on the next step, and the crutches are moved here. Leaning on them, lift your healthy leg one step higher. Descend from the stairs in the reverse order. First, lower the operated leg. Then rearrange the crutches and, supporting them, lower your healthy leg.
Such subtleties are aimed primarily at eliminating pressure on the replaced hip joint and the impossibility of non-compliance with the angle rule (no more than 90 degrees).
Exercise bike
After the patient has learned to sit and walk, exercise on an exercise bike is added to the load. The straightened leg should touch the pedal. To begin, you will need to pedal in reverse side and only after this is successful is it possible to pedal forward.
Balance
It is important to train your balance, trying to stand on one leg. They begin the training with the operated leg, and hold the support with their hand. Then they change legs. Over time, you can make the exercise more difficult by using an elastic band. Balancing will ensure proper functioning of muscles trained by other exercises.
The main thing is not to rush! It is at this time that patients feel that everything is over, the fear has gone, and some even manage to break the rules and recommendations and stop doing gymnastics. Such rash actions will not lead to anything good. The muscles have not yet recovered after the operation, the wounds have not really healed. Strictly follow all rules!
Functional recovery period
 Even when you no longer need crutches or a cane when walking, you still need to train your muscles. It is necessary to completely restore the functions of the artificial joint and promote rapid bone recovery. Only train, overcoming painful sensations, not worth it. It is better to choose the optimal range of motion and perform more over time.
Even when you no longer need crutches or a cane when walking, you still need to train your muscles. It is necessary to completely restore the functions of the artificial joint and promote rapid bone recovery. Only train, overcoming painful sensations, not worth it. It is better to choose the optimal range of motion and perform more over time.
Rules for the postoperative period
In order for everything to recover correctly after the operation and work even better than before the operation, the following rules must be properly followed:
- In a sitting position, the legs should not be closed, they should be slightly spread, moving the operated leg to the side.
- Do not cross your legs under any circumstances.
- Avoid leaning forward.
- Stand up only with a straight back.
- In a sitting position, the knee joints should be slightly lowered, that is, slightly lower than the hip joints.
- When going up and down stairs, hold on to the railing.
Main! Remember that you had a joint replacement.
Video about rehabilitation after endoprosthetics
Rehabilitation after hip replacement at home
 Rebuilding your home has a lot to do with how you prepare your home for your new post-surgery lifestyle. You will need to adapt the house for yourself in advance (even before the operation):
Rebuilding your home has a lot to do with how you prepare your home for your new post-surgery lifestyle. You will need to adapt the house for yourself in advance (even before the operation):
- In the kitchen, everything should be at hand so that you don’t have to bend or stretch forbiddenly;
- The space should allow you to move around with crutches or a cane. To do this, you may need to rearrange the furniture;
- Check your home for safety. Hide the wires, tape off sharp corners - it’s better to do this now than to stumble unsuccessfully after such a serious operation;
- You need to place a special seat with non-slip suction cups in the bathroom and make sure that the handrails you hold on to when getting up are strong;
- At home you will need a high chair or armchair. When sitting, your knees should be lower than your hips.
Rehabilitation after hip replacement depends only on the patient. Don't be lazy and neglect doing exercises
How to properly walk on crutches during rehabilitation
When walking on crutches after hip replacement, you need to keep your back straight and, looking forward, place your foot in front of you or slightly to the side. Bending at the knee is allowed only with weight, and extension on the floor. Walk on crutches for no more than 30 minutes at first.
A set of exercises and physical therapy during the rehabilitation period, it is recommended and developed by the attending physician.
bolezni-spiny.com
Be sure to read other articles:
Exercises after replacement
knee joint
Knee replacement
Smetanin Sergey Mikhailovich
traumatologist - orthopedist, doctor medical sciences
Moscow, st. Bolshaya Pirogovskaya, 6., bldg. 1, metro station Sportivnaya. Registration strictly by phone!!!
Write to us on WhatsApp and Viber
Education and professional activities
Education:
In 2007 he graduated with honors from the Northern State Medical University in Arkhangelsk.
From 2007 to 2009, he completed clinical residency and correspondence postgraduate studies at the Department of Traumatology, Orthopedics and Military Surgery of the Yaroslavl State Medical Academy on the basis of the Emergency Hospital named after. N.V. Solovyova.
In 2010, he defended his dissertation for the degree of Candidate of Medical Sciences on the topic "Therapeutic immobilization of open fractures of the femur"
. Scientific supervisor - Doctor of Medical Sciences, Professor V.V. Klyuchevsky.
Professional activity:
From 2010 to 2011 he worked as a traumatologist-orthopedist at the Federal State Institution "2nd Central Military Clinical Hospital named after P.V. Mandryk".
Since 2011, he has been working in the clinic of traumatology, orthopedics and joint pathology of the First Moscow State Medical University. THEM. Sechenov (Sechenov University), being an associate professor at the Department of Traumatology, Orthopedics and Disaster Surgery.
Conducts active scientific work.
Internships:
April 15-16, 2008 JSC course "AO Symposium Pelvic Fractures"
.
April 28-29, 2011 - 6th educational course "Problems in the treatment of common fractures of the bones of the lower extremities"
, Moscow, State University of Monika named after. M.F. Vladimirsky.
October 6, 2012 - Atromost 2012 "Modern technologies in arthroscopy, sports traumatology and orthopedics"
.
2012 - training course on knee replacement, prof. Dr. Henrik Schroeder-Boersch (Germany), Kuropatkin G.V. (Samara), Yekaterinburg.
February 24-25, 2013 - training course “Principles of total hip replacement”
February 26-27, 2013 - training course "Basics of total hip replacement"
, FSBI "RNIITO im. R.R. Harmful" of the Ministry of Health of Russia, St. Petersburg.
February 18, 2014 - workshop on orthopedic surgery "Endoprosthetics of the knee and hip joints"
,Dr. Patrick Mouret, Klinikum Frankfurt Hoechst, Germany.
November 28-29, 2014 - training course on knee replacement. Professor Kornilov N.N. (RNIITO named after R.R. Vreden, St. Petersburg), Kuropatkin G.V., Sedova O.N. (Samara), Kaminsky A.V. (Kurgan). Subject "Course on ligament balance in primary knee replacement"
, Morphological Center, Yekaterinburg.
November 28, 2015 - Artromost 2015 "Modern technologies in arthroscopy, sports traumatology, orthopedics and rehabilitation"
.
May 23-24, 2016 - congress "Emergency medicine. Modern technologies in traumatology and orthopedics, education and training of doctors"
.
May 19, 2017 - II Congress "Medicine" emergency situations. Modern technologies in traumatology and orthopedics.”
May 24-25, 2018 - III Congress “Emergency Medicine. Modern technologies in traumatology and orthopedics.”
Annual scientific and practical conference with international participation “Vredenov Readings - 2017” (September 21 - 23, 2017).
Annual scientific and practical conference with international participation “Vredenov Readings - 2018” (September 27-29, 2018).
November 2-3, 2018 in Moscow (Crocus Expo, 3rd pavilion, 4th floor, 20th hall) conference"TRAUMA 2018: A multidisciplinary approach."
Associate member of the InternationalNational Society of Orthopedic Surgery and Traumatology (SICOT - French Société Internationale de Chirurgie Orthopédique et de Traumatologie; English - International Society of Orthopedic Surgery and Traumatology). The society was founded in 1929.
In 2015, he was awarded the gratitude of the rector for personal contribution to the development of the university
.
From 2015 to 2018 was an applicant at the Department of Traumatology, Orthopedics and Disaster Surgery of the Medical Faculty of Sechenov University, where he studied the problem of knee replacement. The topic of the dissertation for the degree of Doctor of Medical Sciences: "Biomechanical substantiation of knee arthroplasty for structural and functional disorders"
(scientific consultant, doctor of medical sciences, professor Kavalersky G.M.)
Protection dissertation work
took place September 17, 2018
V dissertation council D.208.040.11
(Federal State Autonomous Educational Institution of Higher Education First Moscow State Medical University named after I.M. Sechenov of the Ministry of Health of Russia (Sechenov University), 119991, Moscow, Trubetskaya St., 8, building 2). Official opponents: doctor of medical sciences, professors Korolev A.V.,Brizhan L.K., Lazishvili G.D.
He is a doctor of the highest qualification category.
Scientific and practical interests: endoprosthetics of large joints, arthroscopy of large joints, conservative and surgical treatment of musculoskeletal injuries.

Tests to be taken before surgery
Before a planned operation, it is necessary to undergo examinations and tests.
The minimum list of analyzes and studies includes:
- General blood analysis- limitation period is 10 days.
- General urine analysis- limitation period is 10 days.
- Biochemical blood test(bilirubin, total protein, AST, ALT, creatinine, urea, C - reactive protein) - statute of limitations is 4 weeks.
- Blood sugar.
- Coagulogram(blood clotting time, bleeding time, INR, prothrombin index, fibrinogen, APTT)
- Blood type and Rh factor.
- Analyzes for infectious diseases
(hepatitis B and C, HIV, syphilis) - statute of limitations is 3 months.
- Electrocardiogram(ECG).
- Fibrogastroduodenoscopy(FGDS).
- Ultrasound examination of the veins of the lower extremities(UZDG) – during operations on the lower extremities.
- Consultation with a therapist
(after 60 years).
The shelf life of other tests before surgery is up to 2-3 weeks.
Check with your attending physician for a list of tests and examinations before surgery, since in some cases, with concomitant pathology, consultation with a cardiologist, endocrinologist, vascular surgeon, or neurologist is additionally necessary; An echocardiographic examination (ultrasound of the heart) is often required.
In addition, before any operation, it is advisable to sanitize foci of chronic infection, that is, visit a dentist, gynecologist, otolaryngologist (ENT doctor) .
All this reduces the risk of postoperative infectious complications.























 An incision is made to the patient at the back approximately at the level of his swimming trunks; it is almost invisible. An experienced surgeon penetrates from behind, without affecting the group of muscles that are important for walking, located on the side of the thigh, and installs the implant. This installation of the prosthesis has a beneficial effect on the restorative function of the hip joint after surgery.
An incision is made to the patient at the back approximately at the level of his swimming trunks; it is almost invisible. An experienced surgeon penetrates from behind, without affecting the group of muscles that are important for walking, located on the side of the thigh, and installs the implant. This installation of the prosthesis has a beneficial effect on the restorative function of the hip joint after surgery.






 The first day the patient should not get out of bed. On the second day, with the help of a doctor - a specialist in physical therapy (physical therapy), the patient is allowed to rise and stand on his feet. Usually, patients are immediately allowed to step on the operated leg with the full weight of their body, but in some cases the attending physician may limit the load on the new joint. All movements of the patient in the postoperative period should be slow and smooth.
The first day the patient should not get out of bed. On the second day, with the help of a doctor - a specialist in physical therapy (physical therapy), the patient is allowed to rise and stand on his feet. Usually, patients are immediately allowed to step on the operated leg with the full weight of their body, but in some cases the attending physician may limit the load on the new joint. All movements of the patient in the postoperative period should be slow and smooth.  4-5 weeks after endoprosthetics, the muscles are already strengthened so much that they become able to withstand more intense loads.
4-5 weeks after endoprosthetics, the muscles are already strengthened so much that they become able to withstand more intense loads. When a joint “becomes unusable” and needs to be replaced, that is, prosthetics, surgeons do the following. In order to get to the joint, 2 large muscles (medium and gluteus maximus), attached to the femur, are released from the fascia. They are moved aside and separated with a blunt instrument, that is, the muscle bundles, although not cut, are separated. Then one mucous bursa is dissected and an incision is made in the gluteus minimus muscle, and then in the articular bursa. The femur is cut at the level of its neck, after which it is removed from the soft tissues of the thigh. An artificial joint is placed and fixed in place of the removed bone. All muscle incisions are sutured.
When a joint “becomes unusable” and needs to be replaced, that is, prosthetics, surgeons do the following. In order to get to the joint, 2 large muscles (medium and gluteus maximus), attached to the femur, are released from the fascia. They are moved aside and separated with a blunt instrument, that is, the muscle bundles, although not cut, are separated. Then one mucous bursa is dissected and an incision is made in the gluteus minimus muscle, and then in the articular bursa. The femur is cut at the level of its neck, after which it is removed from the soft tissues of the thigh. An artificial joint is placed and fixed in place of the removed bone. All muscle incisions are sutured. If rehabilitation after endoprosthetics is not carried out at all or is carried out without the necessary sequence, the injured muscles lose their tone, and scars may form at the incision sites. If the limb is not strained, the ligaments will also heal in a stretched position. This will lead to:
If rehabilitation after endoprosthetics is not carried out at all or is carried out without the necessary sequence, the injured muscles lose their tone, and scars may form at the incision sites. If the limb is not strained, the ligaments will also heal in a stretched position. This will lead to: If a lot of time has passed from the onset of the hip joint disease to the completion of its prosthetics, then rehabilitation should begin even before the operation. This is explained by the fact that due to long-term pain, a person spares his leg, as a result, the muscles of this limb become hypotrophied, which leads to:
If a lot of time has passed from the onset of the hip joint disease to the completion of its prosthetics, then rehabilitation should begin even before the operation. This is explained by the fact that due to long-term pain, a person spares his leg, as a result, the muscles of this limb become hypotrophied, which leads to: Rehabilitation after hip replacement begins from the first minutes after a person wakes up from anesthesia. It consists in:
Rehabilitation after hip replacement begins from the first minutes after a person wakes up from anesthesia. It consists in: Loving relatives should not wait until their elderly, operated parent expresses a desire to begin performing simple exercises - they need to do it themselves, with his limbs. Elderly people often lie in apathy for a long time after stress, one of which is surgery, and may even fall into
Loving relatives should not wait until their elderly, operated parent expresses a desire to begin performing simple exercises - they need to do it themselves, with his limbs. Elderly people often lie in apathy for a long time after stress, one of which is surgery, and may even fall into  This is a very important aspect, and here's why. Vienna
This is a very important aspect, and here's why. Vienna 


 Patients usually stay in hospital for about three weeks. This time is quite enough to teach a person how to lie, sit, walk, climb stairs, and walk on crutches correctly.
Patients usually stay in hospital for about three weeks. This time is quite enough to teach a person how to lie, sit, walk, climb stairs, and walk on crutches correctly. Correct lying position
Correct lying position  It's time to learn how to get out of bed, stand in a stable position and walk. You will need to learn how to perform all these actions independently and, most importantly, safely. It is important to first hear theoretically about how to perform an action correctly and only then perform it correctly. Of course, under the supervision of medical professionals.
It's time to learn how to get out of bed, stand in a stable position and walk. You will need to learn how to perform all these actions independently and, most importantly, safely. It is important to first hear theoretically about how to perform an action correctly and only then perform it correctly. Of course, under the supervision of medical professionals. An important step after endoprosthetics is teaching the patient how to go up and down stairs. This is also a kind of exercise. Not a single person can do without this skill. You can start training when you have mastered proper walking on crutches. It is best to hold on to the railing with the hand on the side of your healthy leg. 1 step - 1 step.
An important step after endoprosthetics is teaching the patient how to go up and down stairs. This is also a kind of exercise. Not a single person can do without this skill. You can start training when you have mastered proper walking on crutches. It is best to hold on to the railing with the hand on the side of your healthy leg. 1 step - 1 step. Even when you no longer need crutches or a cane when walking, you still need to train your muscles. It is necessary to completely restore the functions of the artificial joint and promote rapid bone recovery. Only train, overcoming
Even when you no longer need crutches or a cane when walking, you still need to train your muscles. It is necessary to completely restore the functions of the artificial joint and promote rapid bone recovery. Only train, overcoming  Rebuilding your home has a lot to do with how you prepare your home for your new post-surgery lifestyle. You will need to adapt the house for yourself in advance (even before the operation):
Rebuilding your home has a lot to do with how you prepare your home for your new post-surgery lifestyle. You will need to adapt the house for yourself in advance (even before the operation):