Spanish Fly for two - how they affect libido in women and men
Contents Biologically active additive based on an extract obtained from a beetle with a fly (or fly...
Blood.
Blood and lymph close to it in properties are tissues of the internal environment, characterized by a liquid intercellular substance. blood cells ( shaped elements) make up to 45% of the volume of the entire tissue, while the intercellular substance, or plasma- 55%. The amount of blood in an adult reaches 5-6 liters. Blood performs a number of important functions for the whole organism: respiratory, trophic, excretory, regulatory, homeostatic and protective.
Blood plasma is 90% water. On organic matter, predominantly proteins, account for 9%, and 1% are inorganic substances. Plasma proteins include:
· albumins performing transport functions;
· globulins that carry metals and lipids, and also perform protective functions (immunoglobulins);
· fibrinogen providing blood clotting;
· complement system proteins that protect the body from bacteria.
Most plasma proteins are synthesized by liver cells, with the exception of immunoglobulins secreted by plasma cells in the spleen, lymph nodes and other organs. immune system. Among the inorganic substances highest value have chloride and sodium ions. Inorganic and organic substances of plasma form buffer systems that maintain a constant blood acidity (pH 7.4).
In laboratory practice, for convenience of storage, instead of plasma, blood serum is usually used, which is devoid of fibrinogen and other proteins involved in the formation of a blood clot. The remaining components are present in serum at the same concentrations as in plasma. The concentration of many substances (hemoglobin, glucose, urea, calcium, bilirubin, etc.) is maintained in the blood at the same level, so their determination is used to assess the condition physiological systems organism.
Classification shaped elements(cells) of blood was developed at the beginning of the 20th century, when dyes of complex composition began to be used, which made it possible to stain well both the nucleus and the cytoplasm. In general, all staining methods give similar results, differing only in a finer elaboration of the nucleus (Romanovsky-Giemsa stain) or cytoplasmic granularity (May-Grunwald stain). Therefore, it is often used combined method Pappenheim, combining both dyes.
All formed elements of the blood are divided into red blood cells, or erythrocytes, white blood cells, or leukocytes and platelets, or platelets. There are two types of cells among leukocytes: grainy, or granulocytes, And non-granular, or agranulocytes. The granulocytes are neutrophils, eosinophils And basophils, which differ from each other in the nature of cytoplasmic granularity. belong to agranulocytes monocytes And lymphocytes.
red blood cells have the shape of a biconcave disk with a diameter of 8 and a thickness of 2 microns. The cell is non-nuclear, stains pale yellow or pink color. The cytoplasm of the erythrocyte is filled with the protein hemoglobin, which carries oxygen through the tissues. In addition to transporting oxygen, the erythrocyte also transports the carbonate ion and some other molecules. The number of erythrocytes in 1 microliter is 4.5-5.5 million. A decrease in the number of erythrocytes leads to anemia(anemia), increase - to e rhythremia. These cells mature in the red bone marrow and are destroyed in the spleen. The lifespan of an erythrocyte is about three months.
Neutrophils make up more than half of the total number of leukocytes (about 3-4 thousand per 1 μl). It is a rounded cell 9 μm in diameter with a segmented nucleus and weakly oxyphilic cytoplasm. The number of segments of the nucleus depends on the age of the cell and can reach six. In the cytoplasm of a neutrophil, three types of grains are distinguished. Large basophilic granules are called azurophilic, because the composition of hematological dyes includes azure, which stains these granules. In fact, they are lysosomes. The most numerous is in the neutrophil fine granularity at the resolution limit of the light microscope (250 nm), the color of which cannot be determined, and therefore it is called neutrophilic, or specific. Specific neutrophil granules contain proteins defensins, with which the enveloping occurs ( opsonization) bacterial cells before their phagocytosis. The third type of grains in the neutrophil cytoplasm are peroxisomes.
The functions of neutrophils are associated with protecting the body from bacteria. They are able to attack bacterial cells and violate the integrity of its membrane, as well as phagocytize bacterial cells and destroy them with the help of enzymes of azurophilic granules.
Neutrophils are formed in the red bone marrow and spread throughout the bloodstream, settling on the vascular endothelium. When a focus of inflammation appears, neutrophils pass through the walls of the capillaries and attack bacterial cells, dying in the process. Inactive neutrophils stay in the vascular bed for about a week, and then they self-destruct by apoptosis and are phagocytosed by alveolar macrophages.
Basophils differ from other granular leukocytes in that their cytoplasm is filled with dark purple granules. The cell diameter is 8-10 microns, the number of lobules in the nucleus rarely exceeds 2. Basophil granules have metachromasia, dyed in various shades of blue and purple flowers. Metachromasia is associated with a regular orientation of molecules that exhibit dichroism, absorbing polarized light in different ways. Metachromasia of basophil granules indicates a high regularity of their ultrastructure.
Basophils are contained in peripheral blood no more than 50 cells per 1 μl. However, they can be much more in loose fibrous connective tissue, where they act under the name of mast cells (labrocytes). Basophil granules contain histamine and other inflammatory mediators, which are released from the cell in response to the intake of foreign substances - antigens.
Monocytes- the largest blood cells, their diameter reaches 12-15 microns. The cell nucleus is bean-shaped, it is not divided into segments. In the cytoplasm, a lamellar complex and lysosomes are well developed, there are also inclusions of lipids and glycogen. The cytoplasm is basophilic, without specific granularity, although there is a small amount of azurophilic granules.
The number of monocytes in the blood is 400-500 per 1 µl. They are here in an inactive form. Upon activation, which in higher vertebrates occurs only outside the vascular bed, monocytes turn into macrophages capable of active movement and phagocytosis. Macrophages are able to preprocess and present antigens to other protective cells, stimulate their proliferation and production of antibodies, phagocytize antibody-antigen complexes and dead cells.
Lymphocytes make up to 30% of the total number of leukocytes, occupying the second place in the blood after neutrophils - about 2,000 cells per 1 μl. The cell diameter varies within 7-12 microns. Most of the lymphocyte is occupied by a rounded non-segmented nucleus, a weakly basophilic cytoplasm surrounds it with a narrow asymmetric ribbon. There are few organelles in the cytoplasm. There are small, medium and large lymphocytes. Small lymphocytes belong to the cells that carry out the reactions of cellular immunity. They are distinguished by a cruciform distribution of heterochromatin and a thin layer of cytoplasm around the nucleus. Occasionally, in small lymphocytes, an azurophilic granule can be seen in the cytoplasm. Small lymphocytes make up about 65% of the total number of peripheral blood lymphocytes. Medium lymphocytes, whose proportion in the blood is 20%, have more cytoplasm, their hallmark is a thin light rim around the core. The morphology of the nuclei is also different from that of small lymphocytes; heterochromatin is mainly concentrated in the nucleolemma. Large lymphocytes differ in the core with a notch, the presence of a lamellar complex and several azurophilic granules.
IN functional plan lymphocytes are divided into two types: B-lymphocytes, providing humoral immunity, and T-lymphocytes, which carry out reactions of cellular immunity.
B-lymphocytes mature in red bone marrow. On the surface of these cells there are special receptor proteins that are able to recognize antigens. They are built from an immunoglobulin class M or D (IgM/D) protein. B-lymphocytes, after recognition and activation, turn into plasma cells (plasmocytes), which are producers of antibodies. Thus, B-lymphocytes provide the implementation of the humoral link of the immune response.
T-lymphocytes mature in the thymus (thymus, or goiter, gland). On their surface, they also have receptors (TCRs) capable of recognizing antigens, but they have a different structure than those of B-lymphocytes. T-lymphocytes carry out “double recognition”, simultaneously with the antigen, determining the label of its origin. Some T-cells (cytotoxic lymphocytes) can directly destroy foreign or their own reborn cells, but mainly they control the activity of B-lymphocytes.
T-lymphocytes are represented by three functionally different subpopulations: T-helper cells, T-suppressoritis, and NK cells.
T-helpers, simultaneously with B-lymphocytes recognizing the antigen, stimulate the proliferation and differentiation of B-lymphocytes into plasma cells. T-suppressors also, in parallel with B-lymphocytes and T-helpers, they recognize the antigen, but if the recognition results do not match, they suppress the action of T-helpers. Thus, both B-lymphocytes and T-lymphocytes simultaneously participate in the immune response, but the activity of T-lymphocytes is more regulatory nature. Such a strict control of defensive reactions is due to the fact that in case of erroneous identification, autoimmune disease due to damage own cells and fabrics. Such disorders occur, for example, in rheumatism, when antibodies damage the connective tissue. NK cells unlike other T-lymphocytes, they do not have TCR and therefore are not able to recognize foreign substances. However, with the help of special receptors, they are able to recognize and destroy cancer cells.
Human anatomy and physiology
on the topic of:
The formed elements of the blood. Norm and pathology.
Plan:
1. Red blood cells.
2. Leukocytes.
3. Platelets.
1. Red blood cells.
IN normal conditions in an adult, approximately 25 - 30x10¹² erythrocytes circulate. In 1 µl of peripheral blood of men, there are 4 - 5.5 million erythrocytes, women - 3.9 - 4.7 million.
An erythrocyte is a biconcave cell, i.e. discocyte. Diameter, µm - 7 - 8, volume, µm³ - 90, area, µm² - 140, maximum thickness, µm - 2.4, minimum thickness, µm - 1.
Erythrocytes are highly specialized blood cells. In humans and mammals, erythrocytes lack a nucleus and have a homogeneous protoplasm. The number of red blood cells changes under the influence of external and internal environmental factors (daily and seasonal fluctuations, muscle work, emotions, staying at high altitudes, fluid loss, etc.). An increase in the number of red blood cells in the blood is called erythrocytosis, a decrease is called erythropenia.
Iron metabolism plays an important role in erythropoiesis. The erythroid cells maturing in the bone marrow constantly consume iron for the synthesis of hemoglobin. Some forms of non-hemoglobin iron show up on light microscopy using a special cytochemical stain. Cells containing iron-positive inclusions are called sideroblasts, siderocytes and siderophages.
RBCs are characterized by relatively low level exchange, which provides them with quite a long period life: 120 days. Starting from the 60th day after their release into the bloodstream, a decrease in the activity of various enzymes, primarily hexokinase, glucose-6-phosphate dehydrogenase, fructose-6-phosphate kinase, and glycerinaldehyde-3-phosphate dehydrogenase, increases. This leads to a violation of glycolysis and, as a result, the potential of energy processes in erythrocytes decreases. These changes in intracellular metabolism are associated with cell aging and lead to its destruction. Every day, 200 billion red blood cells undergo destructive changes and die.
The aging of an erythrocyte is accompanied by a change in its configuration, which is reflected in the ratio various forms cells.
Such erythrocytes can be in the form of a dome, a sphere, a deflated ball; there are also single degeneratively changed cells (0.19 ± 0.05%).
According to its structure cell membrane biconcave erythrocyte is the same throughout.
Depressions and bulges can occur and occupy different parts of the membrane.
The cell membrane performs a protective (delimiting) function, separating the cell from the external environment. At the same time, it plays the role of a selective filter through which both active and passive transport of substances into and out of the cell is carried out. external environment. The membrane is the place where the most important enzymatic processes take place and are carried out immune reactions. On its surface, the membrane of a blood cell carries information about the blood type. The membrane has a surface heavy charge, which plays an important role in many processes that ensure the vital activity of the cell. It is directly related to the physicochemical transformations that occur on cell membranes.
The cell membrane can take a spherical shape, then erythrocytes with a larger than normal diameter are described as macrocytes, with a smaller diameter - microcytes. Both those and others are able to hemolyze.
Functions of erythrocytes.
Respiratory the function is performed by erythrocytes due to the hemoglobin pigment, which has the ability to attach to itself and give off oxygen and carbon dioxide.
Nutritious the function of erythrocytes is to adsorb amino acids on their surface, which they transport to the cells of the body from the digestive organs.
Protective the function of erythrocytes is determined by their ability to bind toxins (harmful, poisonous substances for the body) due to the presence on the surface of erythrocytes of special substances of a protein nature - antibodies. In addition, erythrocytes take an active part in one of the most important protective reactions of the body - blood clotting.
Enzymatic The function of erythrocytes is related to the fact that they are carriers of various enzymes. The following were found in erythrocytes: true cholinesterase - an enzyme that destroys acetylcholine, carbonic anhydrase - an enzyme that, depending on the conditions, promotes the formation or breakdown of carbonic acid in the blood of tissue capillaries, methemoglobin - reductase - an enzyme that maintains hemoglobin in a reduced state.
Blood pH regulation carried out by erythrocytes through hemoglobin. Hemoglobin buffer is one of the most powerful buffers, it provides 70-75% of the total buffer capacity of the blood. The buffer properties of hemoglobin are due to the fact that he and his compounds have the properties of weak acids.
Hemoglobin.
Hemoglobin is a respiratory pigment in the blood of humans and vertebrates, it plays an important role in the body as an oxygen carrier and takes part in the transport of carbon dioxide.
The blood contains significant amount hemoglobin: in 1 x 10ˉ¹ kg (100 g) of blood, up to 1.67 x 10ˉ 2 - 1.74 x 10ˉ 2 kg (16.67 - 17.4 g) of hemoglobin is found. In men, the blood contains an average of 140 - 160 g / l (14 -16 g%) of hemoglobin, in women - 120 - 140 g / l (12 -14 g%). Total hemoglobin in the blood is approximately 7 x 10 ˉ1 kg (700 g); 1 x 10ˉ kg (1 g) of hemoglobin binds 1.345 x 10ˉ m 3 (1.345 ml) of oxygen.
Hemoglobin is a complex chemical compound, consisting of 600 amino acids, its molecular weight is 66000 ± 2000.
Hemoglobin is made up of the protein globin and four heme molecules. A heme molecule containing an iron atom has the ability to attach or donate an oxygen molecule. In this case, the valence of iron, to which oxygen is attached, does not change, i.e., iron remains divalent. Heme is the active, or so-called prosthetic, group, and globin is the protein carrier of heme.
IN Lately found that hemoglobin in the blood is heterogeneous. Three types of hemoglobin have been found in human blood, designated as HbP (primitive, or primary; found in the blood of 7–12-week-old human embryos), HbF (fetal, from Latin fetus - fetus; appears in the blood of the fetus at the 9th week of intrauterine development), HNA (from lat. adultus - adult; found in the blood of the fetus simultaneously with fetal hemoglobin). By the end of the 1st year of life, fetal hemoglobin is completely replaced by adult hemoglobin.
Different types of hemoglobin differ in terms of amino acid composition, alkali resistance and oxygen affinity (ability to bind oxygen). Thus, HbF is more resistant to alkalis than HbA. It can be saturated with oxygen by 60%, although under the same conditions the mother's hemoglobin is only 30% saturated.
Myoglobin. Muscular hemoglobin, or myoglobin, is found in skeletal and cardiac muscles. Its prosthetic group - heme - is identical to the heme of the blood hemoglobin molecule, and the protein part - globin - has a smaller molecular weight than hemoglobin protein. Human myoglobin binds up to 14% of the total amount of oxygen in the body. It plays an important role in supplying oxygen to working muscles.
Hemoglobin is synthesized in the cells of the red bone marrow. For the normal synthesis of hemoglobin, a sufficient supply of iron is necessary. The destruction of the hemoglobin molecule is carried out mainly in the cells of the mononuclear phagocytic system (reticuloendothelial system), which includes the liver, spleen, bone marrow, and monocytes. In some blood diseases, hemoglobins have been found that differ in chemical structure and properties from hemoglobin healthy people. These types of hemoglobin are called abnormal hemoglobins.
Functions of hemoglobin. Hemoglobin performs its functions only when it is present in red blood cells. If for some reason hemoglobin appears in the plasma (hemoglobinemia), then it is unable to perform its functions, as it is quickly captured by the cells of the mononuclear phagocytic system and destroyed, and part of it is excreted through the renal filter (hemoglobinuria). Appearance in plasma a large number hemoglobin increases blood viscosity, increases the magnitude of oncotic pressure, which leads to disruption of blood movement and the formation of tissue fluid.
Hemoglobin performs the following main functions. Respiratory function hemoglobin is carried out due to the transfer of oxygen from the lungs to the tissues and carbon dioxide from the cells to the respiratory organs. Regulation of active blood reaction or acid-base state is due to the fact that hemoglobin has buffer properties.
hemoglobin compounds.
Hemoglobin, which has added oxygen to itself, is converted into oxyhemoglobin (HO 2). Oxygen with the heme of hemoglobin forms an unstable compound in which iron remains divalent (covalent bond). Hemoglobin that has given up oxygen is called restored, or reduced hemoglobin (Hb). Hemoglobin attached to carbon dioxide is called carb hemoglobin(HCO). Carbon dioxide with the protein component of hemoglobin also forms an easily decomposing compound.
Hemoglobin can enter into combination not only with oxygen and carbon dioxide, but also with other gases, for example, with carbon monoxide(CO). Hemoglobin combined with carbon monoxide is called carboxyhemoglobin(HCO). Carbon monoxide, like oxygen, combines with the heme of hemoglobin. Carboxyhemoglobin is a strong compound, it releases carbon monoxide very slowly. As a result, carbon monoxide poisoning is very life-threatening.
In some pathological conditions, for example, in case of poisoning with phenacetin, amyl and propyl nitrites, etc., a strong connection of hemoglobin with oxygen appears in the blood - methemoglobin, in which an oxygen molecule attaches to the heme iron, oxidizes it and the iron becomes trivalent (MetHb). In cases of accumulation of large amounts of methemoglobin in the blood, the transport of oxygen to the tissues becomes impossible and the person dies.
The dry matter of an erythrocyte contains about 95% of hemoglobin and only 5% of it is accounted for by non-hemoglobin proteins and lipids, mainly phospholipids. The average value of the dry mass of erythrocytes in men is 36 pg, which exceeds (p< 0,1) величину этого показателя у женщин (33 пг). Хотя сухая масса основного числа клеток (61%) как у мужчин, так и у женщин, колеблется в пределах 30 – 39 пг, эритроцитов с сухой массой от 40 до 50 пг у мужчин больше, а эритроцитов с сухой массой 20 – 30 пг больше у женщин. Такова физиологическая вариабельность эритроцитов по степени насыщения их гемоглобинов.
2. Leukocytes.
Leukocytes, or white blood cells, are colorless cells containing a nucleus and protoplasm. Their size is 8 - 20 microns.
In the blood of healthy people at rest, the number of leukocytes ranges from 6.0x10 9 / l - 8.0x10 9 / l (6000 - 8000 in 1 mm 3). Numerous recent studies indicate a slightly larger range of these fluctuations 4x10 9 / l - 10x10 9 / l (4000 - 10000 in 1 mm 3).
An increase in the number of white blood cells in the blood is called leukocytosis, decrease - leukopenia .
Leukocytes are divided into two groups: granular leukocytes, or granulocytes, and non-grained, or agranulocytes .
Granular leukocytes differ from non-granular ones in that their protoplasm has inclusions in the form of grains that can be stained with various dyes. The granulocytes are neutrophils , eosinophils and basophils . Neutrophils according to the degree of maturity are divided into myelocytes , metamyelocytes(young neutrophils), stab And segmented. The bulk of the circulating blood is segmented neutrophils (51 - 67%). Stab can contain no more than 3 - 6%. Myelocytes and metamyelocytes (young) do not occur in the blood of healthy people.
Agranulocytes do not have specific granularity in their protoplasm. These include lymphocytes and monocytes. It has now been established that lymphocytes are morphologically and functionally heterogeneous. Distinguish T-lymphocytes(thymus-dependent), maturing in thymus, And B-lymphocytes, apparently formed in Peyer's patches (clusters lymphoid tissue in the intestine). Monocytes are probably formed in the bone marrow and lymph nodes.
The number of leukocytes in the blood depends both on the rate of their formation and on their mobilization from bone marrow(depot), as well as from their utilization and migration into tissues (into lesions), capture by the lungs and spleen. These processes, in turn, are influenced by a number of physiological factors, and therefore the number of leukocytes in the blood of a healthy person is subject to fluctuations: it increases towards the end of the day, during physical activity, emotional stress, intake of protein foods, a sharp change in ambient temperature.
Granulocytes
Polymorpho- or segmented granulocytes- These are large cells with a size of 9 - 15 microns, most of which are occupied by the cytoplasm. Their polymorphic core usually contains from 2 to 5 lobules (segments) interconnected by thin threads. The cytoplasm is filled with many dust-like granules, the color of which distinguishes neutrophilic(reddish purple) eosinophilic(bright red) and basophilic(purple blots) granulocytes. Eosinophilic granulocytes are usually slightly larger than neutrophilic ones, while basophilic ones, on the contrary, are smaller than them.
Eosinophilic granulocytes, along with other leukocytes, are capable of phagocytosis. They take part in the detoxification of protein products and play a significant role in the allergic reactions of the body.
The structure of basophils has been studied worse than other granulocytes, since these cells are rarely found in the blood. Their round and polygonal granules with a diameter of 0.15-1.2 microns contain histamine. Consequently, basophils, together with eosinophils, are involved in the allergic reactions of the body, in the metabolism of histamine and heparin. Vasoactive amines from basophils and mast cells may contribute to deposition immune complexes in the walls of blood vessels and, thus, the development of the pathology of immune complexes.
Monocytes.
These are the largest cells normal blood, ranging in size from 12 to 20 microns. The nucleus is large, friable, with an irregular distribution of chromatin; its shape is bean-shaped, lobed, horseshoe-shaped, less often round or oval. In the blood, monocytes circulate for a short time, then they pass into tissues and transform into macrophages.
Monocytes and macrophages are the leading cells of the body's immune response.
Lymphocytes.
The nucleus in the lymphocyte dominates in its mass; it is approximately spherical. Chromatin is usually in the form of coarse compact clumps. Nucleoli are identified using special methods staining and are found in almost all lymphocytes.
With good reason, lymphocytes can be considered as long-lived cells, most of which are in interphase. In lymphocytes, the content of DNA significantly prevails over RNA, which is apparently associated with the specific properties of cells, as well as with the storage of information about antigens. Activation of this information changes the morphological and submicroscopic organization of lymphocytes.
properties of leukocytes.
Leukocytes have a number of important physiological properties: amoeboid mobility, diapedesis, phagocytosis. Amoeba mobility- this is the ability of leukocytes to actively move due to the formation of protoplasmic outgrowths - pseudopodia (pseudopodia). Under diapedesis should understand the property of leukocytes to penetrate through the wall of the capillary. In addition, leukocytes can absorb and digest foreign bodies and microorganisms. This phenomenon, studied and described by I. I. Mechnikov, was called phagocytosis.
Phagocytosis proceeds in four phases: approach, sticking (attraction), immersion and intracellular digestion (phagocytosis proper).
Leukocytes that absorb and digest microorganisms are called phagocytes. Leukocytes absorb not only bacteria that have entered the body, but also dying cells of the body itself. The movement (migration) of leukocytes to the focus of inflammation is due to a number of factors: an increase in temperature in the focus of inflammation, a shift in pH to the acid side, the existence of chemotaxis(the movement of leukocytes towards a chemical stimulus is positive chemotaxis, and from it is negative chemotaxis). Chemotaxis is provided by the waste products of microorganisms and substances formed as a result of tissue breakdown.
Neutrophilic leukocytes, monocytes and eosinophils are phagocyte cells, lymphocytes also have phagocytic ability.
Functions of leukocytes.
One of the most important functions performed by leukocytes is protective. Leukocytes are able to produce special substances - leukins, which cause the death of microorganisms that have entered the human body. Some leukocytes (basophils, eosinophils) form antitoxins- substances that neutralize the waste products of bacteria, and thus have detoxifying property. Leukocytes are capable of producing antibodies - substances that neutralize the action of toxic metabolic products of microorganisms that have entered the human body. In this case, the production of antibodies is carried out mainly by B-lymphocytes after their interaction with T-lymphocytes. T-lymphocytes are involved in cellular immunity, providing a transplant rejection reaction (transplanted organ or tissue). Antibodies can long time be stored in the body component blood, so re-infection of a person becomes impossible. This state of immunity to diseases is called immunity. Therefore, playing a significant role in the development of immunity, leukocytes (lymphocytes) thereby perform a protective function. Finally, leukocytes (basophils, eosinophils) involved in blood coagulation and fibrinolysis.
Leukocytes stimulate regenerative (restorative) processes in the body, speed up wound healing. This is due to the ability of leukocytes to participate in the formation trephons.
Leukocytes carry out enzymatic function. They contain various enzymes (proteolytic - splitting proteins, lipolytic - fats, amylolytic - carbohydrates) necessary for intracellular digestion.
Blood cells are sold as non-specific (inflammation) and specific, including immediate and delayed type reactions (immunity), form of body defense. With any injury or disease, responses involving blood cells can unfold on the surface of epithelial cells lining the body or internal organs, in interstitial fluid, connective tissue, in lymph, or in peripheral blood.
Polymorphonuclear leukocytes and macrophages perform important function: phagocytosis of bacterial and simple eukaryotic pathogens. These cells recognize bacterial or yeast cells by specific receptors located on their surface, usually hydrocarbon structures. Recognition is greatly facilitated by complement (opsonin) and specific antibodies. Antibodies produced by B-lymphocytes work in two ways:
block the biological activity of target molecules (toxin-binding receptors);
Interact with receptors on cells such as macrophages, neutrophils, basophils and mast cells, prompting them to recognize and present the antigen to T-lymphocytes.
The rise of leukocytes to several tens of thousands is described as leukocytosis. It is observed in acute inflammatory and infectious processes, the exceptions are typhoid fever, flu, some stages typhus, measles. The greatest leukocytosis (up to 70-80 thousand) is observed with sepsis. Leukocytosis is usually accompanied by a shift of the leukocyte formula to the left, i.e. the appearance in the peripheral blood of patients with stab and young forms of granulocytes, and in severe cases and exit from the bone marrow of myelocytes, myeloblasts.
A decrease in the number of leukocytes in the blood below 4000 is indicated by the term leukopenia. Most often it concerns neutrophils, i.e. leukopenia appears as neutropenia or agranulocytosis, and may be a manifestation of chronic idiopathic neutropenia, red systemic lupus, rheumatoid arthritis, malaria, salmonellosis, brucellosis, or be a consequence of taking cytostatics and a manifestation of a disease of the blood system. Alcoholism, diabetes, severe shock contribute to the development of neutropenia.
With severe infectious diseases a change in the morphology of neutrophils is possible: toxic granularity, degranulation, vacuolization, etc.
Eosinophilia typical for allergies, helminthiases, but also occurs at the stage of recovery from infectious diseases.
Monocytosis characteristic of tuberculosis, syphilis, brucellosis, protozoal and viral infectious diseases.
lymphocytosis occurs in children with whooping cough, infectious mononucleosis, although it can be a sign of a disease of the blood system. An increase in the number of leukocytes circulating in the peripheral blood to several thousand indicates leukemia. At chronic leukemia such an increase is observed in 98 - 100% of cases, with acute leukemia in 50 - 60%.
Lymphocytopenia develops with primary immunopathology (agammaglobulinemia different types etc.), with diseases of the blood system, Cushing's syndrome, kidney failure. As a specific symptom, lymphocytopenia manifests itself in AIDS, as well as under the influence of radiation, corticosteroid therapy, alkaline drugs and severe edema.
3. Platelets.
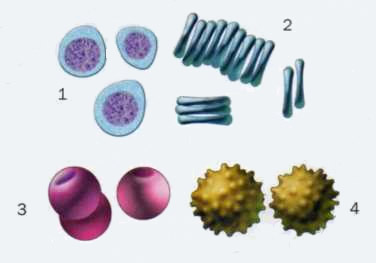
Platelets, or platelets, are oval or rounded formations with a diameter of 2-5 microns. Human and mammalian platelets do not have nuclei. The content of platelets in the blood ranges from 180x10 9 / l to 320x10 9 / l (from 180,000 to 320,000
Peripheral blood platelets are derivatives of bone marrow megakaryocytes. Platelets are fragments of megakaryocytes.
The main forms of platelets in the blood healthy person:
Normal (mature) platelets (87.0 ± 0.13%) are round or oval in shape with a diameter of 3-4 microns; under microscopy, they show a pale blue outer (hyalomere) and central (granulomere) zone with azurophilic granularity;
young (immature) platelets (3.20 ± 0.13%), several large sizes with basophilic cytoplasm and more often centrally located azurophilic granulation (small and medium);
old platelets (4.10 ± 0.21%) can be round, oval, serrated with a narrow rim of dark "cytoplasm" containing abundant coarse granulation, and sometimes vacuoles;
forms of irritation (2.50 ± 0.1%) of large size, elongated, sausage-shaped tailed; The "cytoplasm" in them is blue or pink, azurophilic granularity is scattered or unevenly scattered.
properties of platelets.
Platelets, like leukocytes, are capable of phagocytosis And movement due to the formation of pseudopodia (pseudopodia). TO physiological properties platelets are also adhesiveness , aggregation And agglutination. Under adhesiveness understand the ability of platelets to adhere to a foreign surface. Aggregation- the property of platelets to stick to each other under the influence of various reasons, including factors that contribute to blood clotting. Agglutination platelets (gluing them together) is carried out by antiplatelet antibodies. Viscous platelet metamorphosis- a complex of physiological and morphological changes up to cell decay, along with adhesion, aggregation and agglutination, plays an important role in hemostatic bodily functions (i.e., in stopping bleeding).
Speaking about the properties of platelets, one should emphasize them "readiness" for destruction, and ability to absorb And secrete certain substances, in particular serotonin. All the considered features of platelets determine their involved in stopping bleeding.
Platelet Functions .
1) Take an active part in the process of blood coagulation and fibrinolysis (dissolution blood clot). In the plates, a large number of factors were found that determine their participation in stopping bleeding (hemostasis).
2) They perform a protective function due to agglutination of bacteria and phagocytosis.
3) They are able to produce some enzymes (amylolytic, proteolytic, etc.), which are necessary not only for the normal functioning of the plates, but also to stop bleeding.
4) They affect the state of histohematic barriers, changing the permeability of the capillary wall due to the release of serotonin and a special protein - protein S into the bloodstream.
An increase in the number of platelets - thrombocytosis- is the leading symptom of primary thrombocythemia, although it is also observed in other myeloproliferative diseases (myelofibrosis, myelosclerosis).
Thrombocytosis can accompany chronic processes (rheumatoid arthritis, tuberculosis, primary erythrocytosis, chronic myeloid leukemia, sarcoidosis, granulomatosis, colitis and enteritis), as well as acute infections or hemorrhages, hemolysis, anemia, neoplastic processes. The number of thrombocytes increases after a splenectomy. In cirrhosis with splenomegaly, myelofibrosis, or Gaucher disease, platelets accumulate in an enlarged spleen.
Decrease in the number of platelets - thrombocytopenia- noted during inhibition of the formation of megakaryocytes (leukemia, aplastic anemia, paroxysmal nocturnal hemoglobinuria).
Disturbances in platelet production with thrombocytopenia are manifested in alcoholism and megaloblastic anemia.
Increased destruction and / or utilization of plates occurs in the case of idiopathic thrombocytopenic purpura, post-transfusion, drug-induced thrombocytopenia, neonatal thrombocytopenia, secondary thrombocytopenia in leukemia, lymphoma, systemic lupus erythematosus.
Platelet damage can be induced by thrombin (disseminated intravascular coagulation, complications during childbirth, sepsis, traumatic brain injury).
Dilution of platelets in the bloodstream occurs with massive transfusions of blood and blood substitutes.
Platelet dysfunction can be caused by both genetic and environmental factors.
List of used literature:
1. Kislyak N.S., Lenskaya R.V. Blood cells in children in normal and pathological conditions. Moscow, 1978
2. Shvyrev A.A. "Human Anatomy and Physiology with Fundamentals general pathology". Rostov-on-Don. 2004
3. Lugovskaya S.A., Morozova V.T., Pochtar M.E., Dolgov V.V. "Laboratory hematology", Moscow, 2006.
White blood cell count. In the blood of healthy people under conditions of basal metabolism, the number of leukocytes ranges from 6-8*10 9 /l. They are counted under a microscope in Goryaev's chamber (you will get acquainted with the method in class) or with the help of special electronic counters (hemocytometers).
Morphology and function of leukocytes.
1. Neutrophils . On Romanovsky-stained blood smears, neutrophils have round shape with a diameter of about 12 microns. The size of the cytoplasm significantly predominates over the size of the nucleus. The cytoplasm has a pinkish tint and contains a large number of small bluish-pink granules. The nucleus of mature neutrophils is divided into 3-4 segments connected by thin filaments of chromatin.
The main function of neutrophils is to protect the body from infectious and toxic effects. The participation of neutrophils in defense processes is manifested both by their ability to phagocytosis and digestion of microbes, and by their role in the production of a number of enzymes that have a bactericidal effect. Neutrophils do not produce antibodies, but by adsorbing them on their membrane, they can deliver antibodies to the foci of infection. The phagocytic function of neutrophils is inextricably linked with their ability to amoeboid movement. Both phagocytosis and the movement of granulocytes are associated with energy expenditure, for which the entire set of redox enzymes for ATP synthesis is present in leukocytes. A large amount of glycogen provides the ability of granulocytes to anaerobic glycolysis, which allows them to maintain their functional activity in extremely unfavorable conditions of the inflammatory focus.
The function of granulocytes is not limited to phagocytosis and the transfer of antibodies. During their life cycle, neutrophils secrete whole line substances that have a wide range actions. Some of them have a clear bactericidal activity, others enhance the mitotic activity of cells, improve tissue regeneration, enhance motor activity. The decay products of leukocytes have a stimulating effect on granulocytopoiesis.
Leukocytes carry out their protective function in tissues where their life span can be quite long - up to several months. The duration of the circulation of neutrophils is small, and ranges from 8 hours to 2 days (according to radioactive thymidine).
2. Eosinophils . The diameter of eosinophils ranges from 12 to 15 microns. Their peculiarity is the presence in their cytoplasm of a large number of enzyme-rich granules with a diameter of about 0.2 microns. When stained according to Romanovsky, they take on a yellow-red color and almost completely fill the cytoplasm. The core usually consists of two segments.
Eosinophils have the ability to phagocytosis and amoeboid movement. But their phagocytic activity is much less pronounced than that of neutrophils, so we can assume that phagocytosis is not the main function of eosinophils. Research recent years indicate the undoubted relationship of eosinophils to histamine metabolism. They actively adsorb histamine in places of its maximum accumulation. Thanks to the presence histaminase eosinophils can inactivate histamine. In addition, eosinophils carry adsorbed histamine to the excretory organs - the lungs and intestines. It is well known that eosinophils themselves do not produce histamine, but basophils and mast cells do.
Eosinophils do not produce antibodies. But they adsorb antigens and transfer them to organs rich in plasma and reticular cells (spleen, bone marrow, The lymph nodes), thereby contributing to enhanced production of antibodies. Eosinophils can adsorb many toxic products of a protein nature and destroy them.
The number of these cells in the blood fluctuates throughout the day. Their minimum number is determined at night, the maximum - in morning hours. These daily fluctuations are associated with the activity of the adrenal cortex Increased sympathetic tone nervous system usually leads to eosinophilopenia, vagotonia leads to eosinophilia. Daily fluctuations do not go beyond the physiological norm.
Eosinophilia occurs clinically in many pathological processes most commonly associated with allergies. A decrease in the number of eosinophils is noted with anaphylactic shock, in the acute phase of many infectious diseases, with the introduction of glucocorticoids, with stress.
3. Basophils . The diameter of basophils does not exceed 10 microns. In Romanovsky-stained blood smears, basophils are distinguished by the presence in their cytoplasm of large dark purple granules containing a lot of heparin, histamine and hyaluronic acid. The nucleus has a clawed shape, usually occupying a central position in the cell. The cytoplasm is stained pink.
The function of basophils is reduced to the synthesis of heparin and histamine. Basophils contain about half of all blood histamine. The ability of basophils to synthesize heparin and histamine indicates the direct relationship of these elements to the processes of blood coagulation and flow. allergic reactions, at which degranulation of basophils is always detected.
4.Lymphocytes . Morphological feature lymphocytes, which distinguishes them from other cellular elements of the blood, is the predominance of the size of the nucleus over the size of the cytoplasm. The nucleus is round or slightly oval shape. At conventional methods coloring it is compact. The protoplasm surrounds the nucleus with a narrow rim and is stained with basic colors. By size, small lymphocytes (6-9 microns), medium (10-14 microns), and large (more than 14 microns) are isolated. The majority of circulating lymphocytes belong to the small group. The size is determined by the maturity of the cell - in young it is larger.
The function of lymphocytes is closely related to the processes of immunogenesis. They are involved in the synthesis of beta and gamma globulins of both non-immune and immune nature. The ability to produce antibodies is most pronounced in large and medium lymphocytes. Lymphocytes not only produce antibodies. They have the ability to adsorb circulating antibodies in the blood. Migrating into tissues, lymphocytes deliver antibodies to the foci of inflammation. Lymphocytes also have an antitoxic function. They can adsorb and inactivate toxins of the most diverse origin (bacterial, food, formed during the decay of tissues, etc.).
According to their functional activity and ways of performing a protective reaction, all lymphocytes are divided into two classes: T-lymphocytes(thymus-dependent) and IN- lymphocytes(burso-dependent). The former are responsible for the so-called. cellular immunity, and recognize foreign cells, as they say, in person. The latter provide the so-called. humoral immunity - they sit in the lymphoid organs, react to the antigens brought to them by other cells, and the antibodies they develop enter the bloodstream and spread throughout the body. In addition, among T-lymphocytes, cells are distinguished - suppressors, killers, helpers etc., each of which has its own specific function within the framework of the immune response.
The number of lymphocytes in the blood naturally changes in many pathological processes. Decrease - lymphopenia - permanent and early symptom radiation sickness. It also often develops with the use of glucocorticoids and with stress reactions. Absolute lymphocytosis is characteristic of chronic tuberculous intoxication and lymphatic leukemia.
5. Monocytes . Morphologically, monocytes are well differentiated cells. These are the largest elements of peripheral blood. Their diameter ranges from 13 to 25 microns. When stained according to Romanovsky, significant cell polymorphism is noted, which manifests itself not only in a variety of shapes and diameters, but also in the features of the structure of the nucleus and the color of the cytoplasm. The monocyte nucleus has an irregular oval shape, often bean-shaped with an uneven distribution of chromatin. The protoplasm stains bluish-gray and contains different amount very small azurophilic granules.
Monocytes have the ability for independent amoeboid movement. Their ability to move is much more pronounced than that of lymphocytes. Monocytes are active phagocytes. Due to their mobility, they easily penetrate into the foci of inflammation, where, together with histiocytes, they phagocytose not so much bacteria as decay products of cells and tissues. Monocytes are also able to inactivate the toxins of the inflammatory focus.
Leukocyte formula. When assessing the quantitative changes in leukocytes, it is not so much the changes in their total number that are of decisive importance, but the changes in the percentages different forms leukocytes. The percentage of leukocytes is called the leukocyte formula. The study of the leukocyte formula of a healthy person is not difficult due to a clear morphological characteristics various kinds leukocytes. There are several methods for counting blood smears stained using the Pappenheim or Romanovsky method. You will get to know them in practice.
At healthy individuals the percentage of different types of leukocytes in the blood is relatively constant and looks like this:
eosinophils - 1 - 4%
basophils - 0 - 0.5%
neutrophils -55 - 75% incl.
young - 0 - 1%
stab neutrophils - 2 - 5%
segmented neutrophils - 55 - 68%
lymphocytes - 25 - 30%
monocytes - 6 - 8%.
A moderate deviation from the norm, as well as the appearance of single lymphoid-reticular cells in the blood, is not pathological.
The leukocyte formula, as well as the number of leukocytes, undergoes significant changes during the first years of a person's life. If in the first hours the newborn has a predominance of granulocytes, then by the end of the first week after birth, the number of granulocytes is significantly reduced and their bulk is made up of lymphocytes and monocytes. Starting from the second year of life, there is again a gradual increase in the relative and absolute number of granulocytes and a decrease in mononuclear cells, mainly lymphocytes. The points of intersection of the curves of agranulocytes and granulocytes - 5 months and 5 years. In persons aged 14-15 years leukocyte formula virtually indistinguishable from that of adults.
When evaluating leukograms, great importance should be attached not only to the percentage of leukocytes, but also to their absolute values ("leukocyte profile" according to Moshkovsky). It is quite clear that a decrease in the absolute number of certain types of leukocytes leads to an apparent increase in the relative number of other forms of leukocytes. Therefore, only the determination of absolute values can indicate changes that actually take place.
Factors affecting the number of leukocytes. Although, on average, the blood of a healthy person contains 6-8*10 9 /L, numerous studies indicate a rather large physiological range of their fluctuations (4-10*10 9). There are also age-related changes the number of leukocytes. In newborns during the first day, the number of leukocytes exceeds 20 * 10 9 per l. Subsequently, it rapidly decreases and reaches normal values by 5-6 years.
The constancy of the leukocyte composition of the blood is due to the complex coordination of leukopoiesis and the rate of destruction of leukocytes. Therefore, both violations of the rate of production and changes in the rate of their destruction lead to a change in the number of leukocytes. The quantitative changes in leukocytes arising under these conditions are characterized by stability and duration. They, as a rule, are combined with certain changes in the qualitative composition of leukocytes and violations of their functional activity. So, with most inflammatory diseases naturally develops neutrophilic leukocytosis associated with the activation of granulopoiesis.
A certain value in the occurrence of quantitative changes in leukocytes belongs to their redistribution in the body. Redistributive leukocyte reactions are carried out due to changes in the number of leukocytes deposited in the vessels internal organs mainly in the spleen and lungs. Mature leukocytes deposited in the sinuses of the bone marrow also take part in the implementation of redistributive leukocyte reactions. All of the above fully explains the rapid development of these reactions. Even minimal changes in the functional activity of the body can lead to a redistribution of leukocytes. So, a person in vertical position the number of leukocytes in the blood is slightly higher than in the horizontal. Any physical stress is accompanied by redistributive leukocytosis. The degree of leukocytosis is usually parallel to the intensity of the work being done.
Less natural changes occur in the body when eating. In most healthy people, during the first 15-20 minutes after eating, there is a slight decrease in the number of leukocytes, followed by a moderate increase in their number. The total duration of "digestive leukocytosis" does not exceed 3-4 hours. The number of leukocytes in this case usually remains within the physiological norm.
The group of redistributive leukocyte reactions can also include changes in the number of leukocytes that occur during short-term pain irritation, anesthesia, etc. hallmark redistributive leukocyte reactions is their short duration and the absence of significant changes in the leukocyte formula.
More complex is the pathogenesis of leukocytosis, which often occurs in the second half of pregnancy. At the same time, a shift to the left is often noted in the leukocyte formula, associated with an increase in the percentage of stab neutrophils. It is believed that it depends on the change hormonal balance in pregnant women, which, along with the redistribution of blood, leads to the described changes.
undergoing some kind of changes White blood V different stages adaptation syndrome. In the stage of mobilization, leukopenia is usually noted, associated with a significant decrease in the number of lymphocytes and eosinophils. In the stage of resistance, the composition of the blood usually does not change. With prolonged exposure to an irritant (depletion stage), the number of lymphocytes and eosinophils decreases again with the simultaneous development of neutrophilic leukocytosis. Of certain importance in the development of these changes are glucocorticoids that affect hematopoiesis.
PLATELETS.
The number of platelets in 1 liter of blood in the same person is not stable and varies widely according to a number of physiological factors (gender, age, sleep, physical activity, etc.). The blood contains 2-4*10 11 /l platelets. A significant part of them is deposited in the spleen, liver, lungs and, if necessary, they enter the circulating blood. Various parts of the CNS are involved in the regulation of platelet content.
In women, there are large fluctuations in the number of platelets depending on menstrual cycle, on the 1-2 day of menses, their number decreases by 30-50% Eating usually causes thrombocytosis, similarly physical exercise and dream. The life span of platelets is 8-11 days.
In stained smears, platelets are represented by round or oval formations. When stained according to Romanovsky, in the center of the plate, small grains stained with azure in a dark purple color are determined, the periphery is painted in a homogeneous pale blue color. Sizes range from 2 to 15 microns, with an average of 4 microns.
Upon contact with a foreign surface, platelets lose their shape and begin to spread and release pseudopodial processes, sometimes exceeding the platelet diameter by 5 times. Platelets play a leading role in the process of blood clotting. The marginal standing of platelets in the bloodstream is a kind of barrier that prevents the exit of blood cells from the capillaries, even if the pressure inside the capillary is exceeded (a tourniquet is applied). The active participation of platelets in hemostasis is possible due to their ability to agglutinate and adhere. As a result, at the site of injury blood vessel the so-called. "hemostatic platelet nail", on which a fibrin clot is then superimposed.
Platelets contain many plate coagulation factors, which are both components of the coagulation and fibrinolytic systems, and substances that affect vascular tone. These include:
1 - AS-globulin of platelets;
2 - factor accelerating the conversion of fibrinogen into fibrin;
3 - thromboplastin;
4 - antiheparin;
5 - platelet fibrin;
6 - serotonin;
7 - antifibrinolysin;
8 - retractozyme;
9 - protein S.
The role of platelets in the body is not limited to participation in hemostasis. At present, their immune properties have been proven, antigens have been found in them that differ from the group antigens of erythrocytes. In platelets, agglutinogens of the AB0 system are also detected.
Quantitative and qualitative changes in platelets lead to various pathological conditions. Violations in the blood coagulation system appear not only with insufficient production of platelets, but also when their release into the blood is for some reason difficult. A common form of hemorrhagic diathesis is Werlhof's disease, caused by severe thrombocytopenia, with a violation of blood clot retraction, a significant change in blood clotting time.
Shaped elements- This common name blood cells. The formed elements of blood include erythrocytes, leukocytes and platelets. Each of these classes of cells, in turn, is divided into subclasses.
Since untreated cells that are examined under a microscope are practically transparent and colorless, a blood sample is applied to a laboratory glass and stained with special dyes. Cells vary in size, shape, nucleus shape, and ability to bind dyes. All these signs of cells are called morphological.
erythrocytes(from the Greek erythros - "red" and kytos - "receptacle", "cell") are called red blood cells - the most numerous class of blood cells.
Human erythrocytes are devoid of a nucleus and consist of a framework filled with hemoglobin and a protein-lipid shell - a membrane. The erythrocyte population is heterogeneous in shape and size.
Normally, the bulk of them (80-90%) are discocytes (normocytes) - erythrocytes in the form of a biconcave disc with a diameter
7.5 µm, thickness at the periphery 2.5 µm, in the center - 1.5 µm. An increase in the diffusion surface of the membrane contributes to the optimal performance of the main function of erythrocytes - oxygen transport.
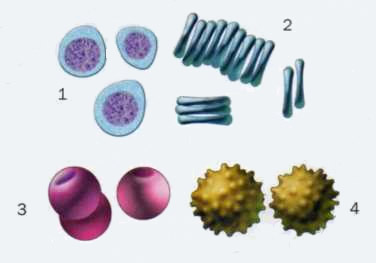
Formed elements of blood in a smear
The specific shape also ensures their passage through narrow capillaries. Since the nucleus is absent, erythrocytes do not need much oxygen for their own needs, which allows them to fully supply oxygen to the entire body.
In addition to discocytes, planocytes (cells with a flat surface) and aging forms of erythrocytes are also distinguished: styloid, or echinocytes (~ 6%); domed, or stomatocytes (~ 1-3%); spherical, or spherocytes (~ 1%).
The filling of red blood cells is hemoglobin - a special protein, thanks to which red blood cells perform the function of gas exchange and maintain the pH of the blood. Normally, in men, each liter of blood contains an average of 130-160 g of hemoglobin, and in women - 120-150 g.
Hemoglobin consists of a globin protein and a non-protein part - four heme molecules, each of which includes an iron atom that can attach or donate an oxygen molecule.
Hemoglobin, which has attached oxygen to itself, turns into oxyhemoglobin, a fragile compound in the form of which most of the oxygen is transported. Hemoglobin that has given up oxygen is called reduced hemoglobin, or deoxyhemoglobin. Hemoglobin combined with carbon dioxide is called carbohemoglobin. In the form of this compound, which also readily decomposes, 20% of carbon dioxide is transported.
Skeletal and cardiac muscles contain myoglobin - muscle hemoglobin, which plays an important role in supplying working muscles with oxygen.
There are several forms of hemoglobin, differing in the structure of its protein part - globin. So, fetal blood contains hemoglobin F, while hemoglobin A predominates in adult erythrocytes. Differences in the structure of the protein part determine the affinity of hemoglobin for oxygen. In hemoglobin A, it is much higher, which helps the fetus not experience hypoxia with a relatively low oxygen content in its blood.
In medicine, it is customary to calculate the degree of saturation of red blood cells with hemoglobin. This is the so-called color index, which is normally equal to 1 (normochromic erythrocytes). Determining it is important for diagnosing various types of anemia. So, hypochromic erythrocytes (less than 0.85) indicate iron deficiency anemia, and hyperchromic (more than 1.1) - about a lack of vitamin B 12 or folic acid.
A number of diseases are associated with the appearance in the blood pathological forms hemoglobin. most famous hereditary pathology hemoglobin is sickle cell anemia: erythrocytes in the patient's blood resemble a sickle in shape. The absence or replacement of several amino acids in the globin molecule in this disease leads to a significant impairment of hemoglobin function.
Erythropoiesis, that is, the process of formation of red blood cells, occurs in the red bone marrow. erythrocytes along with hematopoietic tissue are called red blood sprout, or erythron.
For the formation of red blood cells, iron and certain vitamins are primarily needed.
The body receives iron both from the hemoglobin of degrading erythrocytes and from food: having been absorbed, it is transported by plasma to the bone marrow, where it is included in the hemoglobin molecule. Excess iron is stored in the liver. With a lack of this essential trace element, iron deficiency anemia develops.
For the formation of red blood cells, vitamin B 12, (cyanocobalamin) and folic acid are required, which are involved in DNA synthesis in young forms of red blood cells. Vitamin B 2 (riboflavin) is necessary for the formation of the skeleton of red blood cells. Vitamin B 6 (pyridoxine) is involved in the formation of heme. Vitamin C (ascorbic acid) stimulates the absorption of iron from the intestines, enhances the action of folic acid. Vitamins E (alpha-tocopherol) and PP ( pantothenic acid) strengthen the membrane of red blood cells, protecting them from destruction.
Other trace elements are also necessary for normal erythropoiesis. So, copper helps the absorption of iron in the intestine, and nickel and cobalt are involved in the synthesis of red blood cells. Interestingly, 75% of the total zinc found in human body found in erythrocytes. (Lack of zinc also causes a decrease in the number of leukocytes.) Selenium, interacting with vitamin E, protects the erythrocyte membrane from damage by free radicals (radiation).
The production of erythropoietin is stimulated by any lack of oxygen: blood loss, anemia, heart and lung diseases, as well as being in the mountains. That is why athletes train in mid-mountain conditions, where the oxygen content in the air is less: this allows them to improve their results by accelerating the synthesis of hemoglobin and increasing the delivery of oxygen to the muscles.
The process of erythropoiesis is regulated by the hormone erythropoietin, which is formed mainly in the kidneys, as well as in the liver, spleen, and is constantly present in small amounts in the blood plasma of healthy people. It enhances the production of red blood cells and accelerates the synthesis of hemoglobin. At serious illnesses kidney production of erythropoietin decreases and anemia develops.
Erythropoiesis is activated by male sex hormones, which causes more content red blood cells in men than in women. Inhibition of erythropoiesis is caused by special substances - female sex hormones (estrogens), as well as inhibitors of erythropoiesis, which are formed when the mass of circulating red blood cells increases, for example, when descending from the mountains to the plain.
The intensity of erythropoiesis is judged by the number of reticulocytes - immature erythrocytes, the number of which is normally 1-2%. Mature erythrocytes circulate in the blood for 100-120 days. Their destruction occurs in the liver, spleen and bone marrow. The breakdown products of erythrocytes are also hematopoietic stimulants.
12 Depending on the cause of occurrence, 2 types of erythrocytosis are distinguished.
red blood cells- non-nuclear cells with a diameter of 7 - 8 microns. The shape of erythrocytes in the form of a biconcave disk provides a large surface for free diffusion of gases through its membrane. The total surface of all erythrocytes in the circulating blood is about 3000 m 2 .
main feature erythrocytes - the presence of a respiratory pigment (red) hemoglobin (Hb), which makes up about 90% of the substance of erythrocytes, and 10% are minerals- salts, glucose, proteins and fats. Hemoglobin is a complex chemical compound, the molecule of which consists of a protein (heme carrier) and an active iron-containing part - heme, which has the ability to easily combine with oxygen and just as easily give it away. Combining with oxygen, it becomes oxyhemoglobin (HbO), and giving it away, it turns into reduced (reduced) hemoglobin. And the norm in the blood of women contains 120-140 g / l Hb, in men - 135 - 155 g / l . A decrease in the amount of Hb (anemia) is observed with intoxication, bleeding, lack of folic acid, iron, vitamin B.m, etc.
The number of red blood cells in the blood of men is 5 x 10 | 2 / l, in women 4.5 x 10 12 / l. In the process of blood movement, erythrocytes do not settle, as they repel each other, since they have the same (negative) charges. When blood settles in a capillary, erythrocytes settle to the bottom, since the specific density of erythrocytes is higher than the density of plasma. The erythrocyte sedimentation rate (ESR) is expressed in mm of the height of the plasma column above the erythrocytes per unit of time; V normal conditions in men it is 4-8 mm in 1 hour, in women it is 8-12 mm in 1 hour. ESR depends on the number of erythrocytes, the magnitude of the charge, the protein composition of the plasma, etc.: during pregnancy it increases to 30 mm / h, with infectious, inflammatory and malignant diseases- up to 50 mm/h and more.
Functions of red blood cells: binding and transfer of oxygen from the lungs to organs and tissues, binding of toxins.
Leukocytes according to functional and morphological features, they are ordinary cells containing a nucleus and protoplasm. They have amoeboid mobility and can pass through intact capillary endothelium. Leukocytes are heterogeneous in their structure: in some of them, the protoplasm has a granular structure (granulocytes), in others there is no granularity (agranulocytes). Granulocytes make up 65-70% of all leukocytes and, depending on the ability to stain with neutral, acidic or basic dyes, are divided into neutrophils, eosinophils and basophils, respectively.
Agranulocytes make up 30-35% of all white blood cells and include lymphocytes and monocytes. The functions of various leukocytes are varied.
Percentage different forms of leukocytes in the blood is called the leukocyte formula (see below). The total number of leukocytes and the leukocyte formula are not constant. An increase in the number of leukocytes in peripheral blood is called leukocytosis, and a decrease is called leukopenia (with some infectious diseases, exposure to radiation, some drugs). Leukocytosis can be physiological (after eating, during pregnancy, muscle exertion, pain, stress) and pathological (with infections and inflammatory processes). The life span of leukocytes is 7-10 days.
Neutrophils make up 60-70% of all leukocytes and are cells that protect the body from bacteria and their toxins. Penetrating through the walls of capillaries (diapedesis), neutrophils enter the interstitial spaces, where phagocytosis is carried out.
Eosinophils(1-4% of the total number of leukocytes) adsorb antigens, many tissue substances and toxins of a protein nature on their surface, destroying and neutralizing them. Eosinophils are involved in preventing the development of allergic reactions, as they have an antihistamine effect.
Basophils make up no more than 0.5% of all leukocytes and carry out the synthesis of heparin, which is part of the anticoagulant blood system; participate in the synthesis of a number of biologically active substances and enzymes (histamine, serotonin, RNA, phosphatase, lipase).
Lymphocytes(25-30% of all leukocytes) do not have amoeboid movement. They are playing essential role in the processes of formation of the body's immunity, and also actively participate in the neutralization of various toxic substances.
The main factor of the immunological system of the blood are T and B-lymphocytes. T-lymphocytes primarily play the role of a strict immune controller. Having come into contact with any antigen, they remember its genetic structure for a long time and determine the program for the biosynthesis of antibodies (immunoglobulins), which is carried out by B-lymphocytes.
B-lymphocytes, having received a program for the biosynthesis of immunoglobulins, turn into plasma cells, which are antibody factories.
T-lymphocytes synthesize substances that activate
phagocytosis and protective inflammatory responses. They are watching
genetic purity of the organism, preventing engraftment
foreign tissues, activating regeneration and destroying dead or mutant (including tumor) cells of your own body. T-lymphocytes play the role of regulators of the hematopoietic function, which consists in the destruction of foreign stem cells in the bone marrow. Lymphocytes are able to synthesize beta and gamma globulins, which are part of antibodies. Unlike other leukocytes, they not only penetrate tissues, but are also able to return back to the blood, and live not for several days, but for decades.
Monocytes(4-8%) are the largest white blood cells, which are called macrophages. They have the highest phagocytic activity in relation to the decay products of cells and tissues, neutralize toxins formed in the foci of inflammation. Monocytes are involved in the production of antibodies. Macrophages, along with monocytes, include reticular and endothelial cells of the liver, spleen, bone marrow and lymph nodes.
platelets are small, non-nuclear platelets irregular shape diameter 2-5 microns; possess amoeboid mobility. Despite the absence of a nucleus, platelets have an active metabolism and are the third independent living blood cells. Platelets play a leading role in blood clotting. The normal content of platelets is 250 x 10 9 l.
The lack of platelets in the blood - thrombopenia - is observed in some diseases and is expressed in increased bleeding.