What is possible and not possible during the Nativity Fast?
In 2018, the Nativity Fast will begin on November 28. During this period, Orthodox believers prepare to celebrate Christmas...
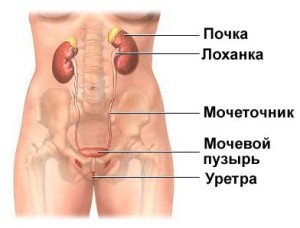
Urethritis is an inflammatory disease in which the urethra (or urethra) is affected. Urethritis, the symptoms of which appear against the background of exposure to viruses or bacteria that provoked this inflammation, in its own course may correspond to the nature of infectious process or a non-infectious process.
The urethra itself is the channel through which urine is discharged outward from the bladder. Urethritis is predominantly diagnosed in those with active sex life young patients, and it is the sexual route of transmission that determines greatest number patients seeking appropriate medical care.
Symptoms of urethritis in women, by the way, are sometimes extremely difficult to distinguish from the symptoms that appear with cystitis. Actually, cystitis in women, which, as the reader probably knows, is a disease accompanied by inflammation of the bladder, is often a companion to urethritis, due to which the identification of both actual variants of the disease is somewhat complicated. The reason for this is the similar nature and symptoms. The difference is the actual localization of the inflammatory process and the symptoms that appear in both cases - the main symptoms of cystitis are based on increased urination, while with urethritis, urination is only combined with certain unpleasant sensations. However, one cannot deny the possible relationship between both of these diseases, because urethritis can develop against the background of cystitis, or, conversely, serve as the basis for its future development. These variants are caused by the ascending or descending route of infection.
The disease is not life-threatening, but its appearance, as one might assume, causes a certain kind of adjustment in life during the period of manifestation.
It should immediately be noted that due to the peculiarities of the location of the urethra, which is somewhat shorter in women, urethritis in men develops almost unhindered. The urethra in men has several physiological narrowings and bends, which determines their greater predisposition to urethritis. Returning to the characteristics of the urethra in women, it remains to be noted that, as is already clear from the comparison, it is straight and short enough, which ensures practical washing away of the actual infection when urinating.
So to speak, in a “pure” form, urethritis is detected in patients extremely rarely. The “pure” form, in particular, means such a course of this disease in which the inflammation typical for it does not occur in the genitals. The first symptoms of urethritis require consultation with a doctor. The reason for this is the possible worsening of the course of this disease in the future, which, in turn, may manifest itself in a slightly different form. Thus, exposure to viruses or pathogenic bacteria against the background of urethritis, with such aggravation, it can provoke infection of the prostate gland or epididymis in men.
Basically, urethritis develops as a result of infection with one or another sexually transmitted disease, which, as already noted, is facilitated by the main method of infection - sexual contact. Also, a violation of the rules provided for personal hygiene acts as a provoking factor for urethritis. Besides stated reasons, which, however, happens somewhat less frequently, the introduction of microbes into the urethra is also considered possible, which occurs as a result of several other reasons. In particular, in this case it means inflammation of the organs located above, or the introduction of microbes through the lymphatic and blood vessels from foci of inflammation relevant to the body. Examples of such foci of inflammation include inflammatory processes in dental diseases, inflammation of the tonsils (which occurs with tonsillitis), etc.
Urethritis can be gonococcal (specific urethritis) or, accordingly, non-gonococcal (nonspecific urethritis); there is also a more expanded version of its classification.

Structure female organs: urethra (urethra)
Causes of urethritis we are in in general terms highlighted slightly higher. Upon closer examination, the reasons are determined based on the classification compliance.
First of all, urethritis can be specific or nonspecific.
Specific urethritis diagnosed in cases where it is provoked by infections that are transmitted through sexual contact. Such infections include herpes virus, gonococcus, ureaplasma, and trichomonas. Somewhat less commonly, these are mycoplasma, chlamydia, gardnerella, etc. Specific urethritis is similarly defined as gonococcal urethritis (based on the nature of one's own emergence, as can be understood from the definition of this form).
As for the next form, which is nonspecific urethritis, then opportunistic microflora is considered here as an influencing factor. Examples include staphylococci and streptococci, Escherichia coli, various options varieties of mushrooms.
Specific urethritis also defines a separate group within them, this non-gonococcal urethritis. This group is characterized by the fact that urethritis in it is provoked by various types of viruses and infections, but with the exception of gonococci. In turn, this group defines two other forms of urethritis, and this infectious urethritis or non-infectious urethritis. And if with infectious urethritis, in principle, no questions arise regarding the specifics of its occurrence, and it is determined on the basis of the name itself, then non-infectious urethritis, of course, can provoke the corresponding interest of the reader.
The basis for the development of non-infectious urethritis can be physical damage to the urethra. For example, this could be a blow or a diagnostic procedure that led to such a lesion, thermal or chemical exposure. In accordance with the traumatic nature of non-infectious urethritis, it is also defined as traumatic urethritis. Non-infectious urethritis, among other things, can also be allergic. Allergic urethritis, According to the specifics of allergies, it can act as a reaction of the body that occurs in response to food, drugs or other allergens. In some cases, urethritis is diagnosed in patients with diabetes mellitus and other types of metabolic disorders.
But these options do not complete our classification. In addition to the options already listed, urethritis can be primary or secondary. Primary urethritis is an independent disease that develops directly in the urethra, while secondary urethritis is the result of a complication of a particular disease. Infection in secondary urethritis occurs mainly from the bladder, vagina or prostate gland, etc.
Based on the considered classification options, urethritis, in accordance with the reasons that provoked it, can also be divided into two groups, and this venereal urethritis And non-venereal urethritis. As has already been highlighted, urethritis can be gonorrheal or non-gonorrheal, and both of these options can be classified as venereal urethritis, provided that the route of infection was sexual.
Can provoke urethritis urolithiasis disease, which is caused by the movement of sand or stone along the urethra, as a result of which its walls are damaged. Significant causes of urethritis can also be noted: physical exercise, characteristics of sexual life (excessively active sex life, or, conversely, inconsistent sex life). Certain Products Also contribute to the development of urethritis, and these are salty foods, sour, spicy or pickled foods. In reality, there can be many factors, and those that we have listed are only the basis.
The duration of the incubation period of the disease (which is the time interval between infection and the appearance of the first symptoms) is determined based on the specific pathogen that provoked urethritis. On average, the incubation period for gonococcal urethritis is about 3-10 days after infection occurs (contact itself), although a shortened version is not excluded. Thus, certain strains provoke the development of urethritis already 12 hours after contact. However, the manifestation of this disease even 3 months after this cannot be ruled out - here, of course, we are talking about a different type of strain that determines such a scenario.
The main manifestation characterizing the course of urethritis is purulent discharge appearing from the urethra. Such discharge may be either yellow-green or pale yellow.
Symptoms of acute urethritis are characterized by itching, burning and pain; all these manifestations are noted at the very beginning of urination, again, by the appearance of purulent discharge. The edges on the side of the external opening of the urethra begin to become inflamed and, as the process progresses, stick together. At the same time, it is possible to develop urethritis without the concomitant appearance of purulent discharge, but with the listed symptoms that directly accompany the act of urination.
Urethritis, the symptoms of which appear in a rather severe form in men, manifests differently in women. Thus, the symptoms of urethritis in women are characterized by less severity, and in some cases they may not be detected at all.
Types of urethritis are characterized by their own characteristics of the course, despite the characteristics already indicated, depending on the stage of the course, several typical forms are determined, we will dwell on them in more detail.
Acute urethritis: symptoms
This variant of urethritis is accompanied by characteristic painful urination and burning sensation. These symptoms are also combined with copious discharge, which, as already noted, appears from the urethra. The lips of the external opening of the urethra turn red, swelling is noted, and the inflammatory process is concentrated in the area of the wall of the urethra. Slight pressure leads to the expiration of purulent discharge. After a night's sleep, purulent spots can be found on your underwear. Feeling the urethra allows you to identify some of its density.
In general, the sensations that a patient experiences with urethritis are characterized by the scale of the inflammatory process within the urethra (this is posterior urethritis, anterior urethritis, or complete urethritis), and the relevance of complications is also taken into account. Thus, some patients may experience burning or itching in the area of the urethra, while others especially experience pain during urination.
If an acute variant of torpid urethritis (a low-symptomatic form of this disease) is considered, then the urge to urinate is frequent, pain is noted in the urethral area, and body temperature rises. In this case, the completion of the act of urination is the appearance of a minimal amount of bloody discharge, which is defined as terminal hematuria. There is also swelling of the urethra. In general, the course of torpid urethritis, if we are not talking about its acute form, is characterized by its own monotony, such a course does not have sharp boundaries, as a result, it transitions to chronic form course of gonorrhea.
Subacute urethritis: symptoms
This form is characterized by a gradual reduction in swelling and pain in the urethra. Purulent discharge is either scanty or disappears altogether. In some cases, the presence of discharge in the morning is allowed (it looks like a crust, due to which the external opening in the urethra sticks together). The urine also changes: it becomes more transparent, and minor purulent threads are noted in its composition.
Chronic urethritis: symptoms
The transition to a chronic form occurs when therapy for the disease is ineffective or in the absence of proper treatment as such. The appearance of complaints (exacerbation of urethritis) in this case is preceded by the influence of provoking factors, against the background of which a certain amount of purulent discharge appears. Such factors include hypothermia, the patient’s consumption of alcohol, etc. Basically, the symptoms of chronic urethritis coincide with the manifestations characteristic of the torpid form of urethritis, which we previously identified. The course of the disease can be long-term, which means not only months, but also years, which ultimately may lead to a visit to the doctor (if this was done earlier, before the disease progressed to this form). A long course of this form of urethritis can provoke urethral stricture, in which the urethra in the lumen begins to narrow, which is why urination is accompanied by a change in the stream of urine (it becomes weak) and pain.
Total urethritis: symptoms
The peculiarity of this form of urethritis is that the urethra is completely exposed to inflammatory damage. The symptoms of total urethritis are characterized by similarities with the symptoms of prostatitis. In acute total urethritis, the urge to urinate is uncontrollable, and completion of urination is accompanied by pain. There are bloody and purulent components in the urine.
Diagnosis is based on a physical examination of the patient if he has symptoms indicating possible urethritis. The examination is carried out 1-3 hours after the last act of urination. The diagnosis of acute urethritis or chronic urethritis is established on the basis of swelling and redness of the urethra, as well as on the basis of purulent discharge.
In the future, a Gram smear is done if there is a suspicion of the relevance of gonorrheal urethritis. Diagnosis of the disease is also supported by the results of a urine test by detecting leukocytes in the sediment, analysis of scrapings of the urethra and vagina (the presence of chlamydia is determined). If necessary, a scraping from the rectal area can be done.
Definition of measures drug therapy based on the characteristics of the nature of the disease. The main treatment measures are rinsing using antiseptic drugs, aimed directly at the urethral area, antibiotics can also be used. Efficacy in the treatment of urethritis is determined by the use of erythromycin and tetracyclines. Additional effect is achieved through physiotherapy procedures (warming applications, electrophoresis, etc.), local treatment (for example, sitz baths based on herbal decoction), taking immunostimulants and immunomodulators.
Diet during treatment is mandatory. It specifically excludes salty, smoked and spicy foods and alcohol. In the acute stage of the disease, the diet is based on products of lactic acid origin, and drinking plenty of fluids is also recommended. The influence of negative provoking factors (physical overload, hypothermia) is excluded; restrictions also apply to sexual activity during this period.
If urethritis is not treated, there is a risk of developing already noted prostatitis (in chronic form), and in some cases, epididymitis, and this disease subsequently becomes the cause of infertility (obstructive form). Vesiculitis may also develop.
The main method of preventing urethritis is the implementation of the barrier method, which consists of contraception using condoms, which is especially important during sexual intercourse with non-regular partners. Also important in the prevention of gonorrhea is proper hygiene measures.
If you suspect the relevance of urethritis, you should visit a venereologist; in case of nonspecific urethritis, the patient is referred to a urologist.
Urethritis is inflammation of the mucous membrane of the urethra.
Urogenital bacterial infections represent one of the most pressing problems of modern urology, venereology, gynecology and other branches of medicine.
Information about their frequency is contradictory, which is due to the dependence of this indicator on the characteristics of the population being examined, the place and time of research, and the level of laboratory diagnostics.
N34.1 Nonspecific urethritis
N34 Urethritis and urethral syndrome
N34.2 Other urethritis
N37.0* Urethritis in diseases classified elsewhere
Manifold clinical forms nonspecific urethritis is caused by various etiological factors. The occurrence of a significant part of them is associated with infection. According to modern concepts, urethritis can be caused by microorganisms usually present in the microbial flora lower sections genital tract or entering them from the outside during sexual intercourse or when the composition of the vaginal and urethral microflora changes in favor of virulent microorganisms.
Bacterial urethritis is a disease in which bacteria of “banal” microflora of various genera are detected: Esherichia coli, Klebsiella, Enterobacter, Serratia, Proteus, Citrobacter, Providenci, Staphylococcus aureus. The latter predominates and plays a role in the occurrence of urethritis not only as a monoculture, but also in microbial associations with which the persistent course of the disease in such patients is associated.
The most common causative agents of urethritis in men are Chlamydia trachomatis and Neisseria gonorrhoeae. However, in a significant proportion of patients with clinical urethritis (up to 50%), these microorganisms are not detected. In such cases, non-chlamydial non-gonococcal urethritis is diagnosed, which, however, is presumably classified as an STI. Although, despite numerous studies, the predominant role of any microorganism in the development of non-chlamydial non-gonococcal urethritis has not yet been proven.
The high frequency of detection of Chlamydia trachomatis in patients with urogenital gonorrhea has led to recommendations for the prophylactic administration of antichlamydial drugs to patients suffering from gonorrhea.
Causing not only nonspecific urethritis, mycoplasmas can cause kidney disease and urinary tract. Research confirms this. that infection caused by Mycoplasma genitalium is quite common among men who seek outpatient care with symptoms of urethritis. In patients with clinical symptoms of non-chlamydial non-gonococcal urethritis, M. genitalium was detected in 25% of cases. In patients without symptoms of urethritis, the frequency of isolation of M. genitalium was significantly lower and amounted to only 7% (p = 0.006). The frequency of M. genitalium isolation among men with gonococcal and chlamydial urethritis was 14 and 35%, respectively.
At the same time, the role of other intracellular pathogens, in particular Ureaplasma urealyticum, in the development of postgonococcal urethritis still remains unclear.
Trichomonas urethritis takes 2-3rd place after gonorrhea and chlamydia. In most cases, the disease occurs without clearly defined clinical symptoms and any features that distinguish it from urethritis of other etiologies. The causative agent of trichomoniaea is classified as a member of the genus Trichomonas, grouped into the class Flagellates. Of all types of Trichomonas, Trichomonas vaginalis is considered pathogenic. In women, it lives in the urethra and vagina, in men - in the urethra, prostate and seminal vesicles. In 20-30% of patients, trichomonas infection can occur as a transient and asymptomatic carriage
The causative agents of viral urethritis include herpes simplex viruses type 2 (genital) and genital warts. In recent years, there has been a tendency towards their widespread distribution. Both viruses cause disease only in humans. Infection occurs through close, intimate contact. At the same time, you can become infected from an infected patient both in the presence of symptoms of the disease and in their absence. Primary infection is often accompanied by severe symptoms, after which the virus enters a latent state. Repeated exacerbation of the disease is observed in 75% of patients.
Fungal infections of the urethra most often occur in patients with immune and endocrine disorders (diabetes) or as a complication of long-term antibiotic therapy. Fungal infections include candidiasis of the urethra, the cause of which is yeast-like mushroom Candida. It is found in the discharge from the urethra in the form of a large amount of pseudomycelium in thick, dense mucus. In women, candidal urethritis occurs due to damage to the reproductive system by Candida due to wide application antibacterial agents. In men, candidal urethritis is isolated, and infection occurs through sexual contact.
Gardnerella lesions of the urethra occupy a certain place among sexually transmitted diseases. In recent years, infections caused by Gardnerella have increasingly attracted the attention of researchers.
Gardnerella urethritis is currently receiving attention from various specialists who recognize the participation of Gardnerella in the development of urethritis in women. so do men. The disease develops as a result of infection of the vagina by Gardnerella vaginalis, a nonmotile gram-negative rod that is sexually transmitted. Mixed infection with chlamydia, ureaplasma, protozoa, fungi and anaerobic microorganisms is often noted.
With the development of nonspecific urethritis, deterioration plays a significant role among the risk factors. general condition body, alcohol intake, insufficient physical activity, as well as venous congestion in the submucosal layer of the urethra, often caused by sexual excesses.
Autoimmune processes play a significant role in the pathogenesis of nonspecific urethritis, especially with mixed specific and nonspecific infections, which often leads to low effectiveness of antibiotic monotherapy and a long, persistent course of the disease.
Infectious urethritis can be transmitted sexually and, while the incubation period is well known for gonorrhea and Trichomonas urethritis, for most nonspecific urethritis it has not been definitively established. Its duration ranges from several hours (allergic urethritis) to several months (with viral and other urethritis). Clinically, according to the severity of the signs of the disease, three main forms of urethritis are distinguished:
Symptoms of urethritis are characterized by the following:
Acute urethritis is characterized by an abundance of discharge from the urethra on the head of the penis; it can shrink into yellowish crusts. The sponges of the urethra become bright red, swollen, and the mucous membrane of the urethra may turn outward somewhat.
On palpation, the urethra is thickened and painful, which is especially noticeable with periurethritis. The affected large paraurethral glands are found in the form of small formations similar to large grains of sand. Subjective disorders are sharply expressed - burning and pain at the beginning of urination, its frequency. The first portion of urine is cloudy and may contain large threads that quickly settle to the bottom of the vessel. In case of damage to the posterior part of the urethra clinical picture changes - the amount of discharge from the urethra decreases, the frequency of urination increases sharply, at the end of urination a sharp pain and sometimes blood appears.
The symptoms of torpid and chronic urethritis are approximately the same. Subjective symptoms of urethritis are mild, characterized by discomfort, paresthesia, itching in the urethra, especially in the area of the scaphoid fossa. As a rule, there is no free discharge from the urethra, but there may be sticking of the urethral sponges. In some patients, symptoms of urethritis are negative emotional coloring associated with individual characteristics experiences of the disease itself. In the first portion of urine, which is usually transparent, small threads may float and settle to the bottom.
With the above symptoms in the first 2 months, urethritis is called torpid, with a further course - chronic.
IN clinical practice It is customary to classify urethritis into two large groups.
Residual, psychogenic, iatrogenic inflammation of the urethra is also possible.
In addition, bacterial urethritis is often divided into gonococcal and non-gonococcal (non-specific). However, most researchers do not currently use this classification. Separately, we should highlight urethritis caused by nosocomial infection, which can be accidentally introduced into the urethra during various manipulations:
With transient urethritis, we are talking about the lightning-fast course of urethritis during the passage of a urogenital latent infection (chlamydia, ureaplasma, mycoplasma, gardnerella, much less often - genital herpes virus type 2) during infection of the patient after sexual intercourse with a sick partner. In such patients, clinical signs are subtle. Such patients are identified among those who have had sexual intercourse with a dubious partner without a condom. As a rule, these are men with significant sexual experience who have been treated and fully recovered from hidden and even sexually transmitted diseases.
In recent decades, there has been an increase in the number of people suffering from nonspecific urethritis, the number of which in relation to all other types of urethritis has increased, according to various venereological clinics, by 4-8 times.
Basic methods for diagnosing urethritis:
The initial and one of the most critical stages of the etiological diagnosis of infections of the genitourinary system is the collection and transportation of biological material.
Basic rules for taking material from women:
Basic rules for collecting material from men:
In torpid and chronic forms of urethritis, material for research can be obtained by carefully scraping the mucous membrane of the anterior urethra with a Volkmann spoon.
The bacterioscopic method includes the study of secretions from the urethra using staining (Gram, Romanovsky-Giemsa, etc.) and is intended to identify microbes (primarily gonococcus) and protozoa. To detect trichomonas, a study of native preparations is used
This method makes it possible to identify, in addition to microbes and protozoa, cellular elements - leukocytes, epithelial cells, as well as various variants of microorganism associations. In addition to the detection of the direct causative agent of urethritis, it is also indicated by the detection of 5 or more polymorphonuclear leukocytes in the field of view.
The bacterioscopic method not only makes it possible to determine the presence of an infectious process in the urethra, but helps to determine its etiology, as well as further tactics for managing the patient. In the absence of signs and symptoms of urethritis or polymorphonuclear leukocytes during bacterioscopic examination, therapeutic and sometimes additional diagnostic measures are postponed.
In clinical practice, to diagnose gonorrhea, in addition to the bacterioscopic method, bacteriological methods are used, less often immunofluorescence, immunochemical and serological tests. Bacterioscopy of smears from the urethra reveals gram-negative diplococci. located intracellularly, characterized by polychromasia and polymorphism, as well as the presence of a capsule. Bacteriological research consists of isolating a pure culture of gonococcus on meat peptone agar.
The diagnosis of Trichomonas urethritis is made on the basis of clinical signs of the disease and the detection of Trichomonas in the test material. For this purpose, bacterioscopy of an unstained fresh preparation and examination of a Gram-stained specimen are carried out; bacteriological examination is less often performed using solid nutrient media.
Diagnosis of Gardnerellosis urethritis is based on bacterioscopic examination of native preparations, as well as Gram-stained preparations. In native preparations, flat epithelial cells are found, to the surface of which gardnerella are attached, giving them a characteristic “peppered” appearance. This is considered a pathognomonic sign of gardnerellosis. The cytological picture in stained smears is characterized by the presence of individual leukocytes scattered in the field of view, a significant number of small gram-negative rods located on epithelial cells.
Clinical manifestations of urethritis, in which various variants of staphylococci, streptococci, coli, enterococci and some other opportunistic microorganisms, depend on the location pathological process and cannot be differentiated from infections caused by other pathogens. In these cases, a multi-glass urine sample is considered mandatory. Bacteriological methods make it possible to determine the number of pathogens in 1 ml of fresh urine, their species and type, as well as sensitivity to antibiotics.
TO clinical methods studies also include urethroscopy, which is indicated to clarify the nature of damage to the mucous membrane of the urethra, complications of prostatitis, vesiculitis, etc.
The basic principles for diagnosing chlamydial infection are the same as for other bacterial diseases. Test procedures include:
The bacterioscopic method for detecting chlamydia involves identifying the morphological structures of chlamydia in the affected cells. Currently used rarely due to low sensitivity (10-20%).
To detect chlamydia antigens in clinical samples during bacterioscopic studies, both direct and indirect immunofluorescent methods can be used. In direct immunofluorescence, the drug is treated with specific mono- or polyclonal antibodies labeled with fluorescein. In the indirect immunofluorescent method, the drug is treated first with an immune serum containing unlabeled anti-Chlamydial antibodies, and then with an anti-species fluorescent serum. Viewing is carried out using a fluorescent microscope. The sensitivity of this bacterioscopic examination is 70-75% for cervical mucus in women and 60-70% for scrapings from the urethra in men.
The bacteriological method for diagnosing chlamydial infection is based on isolating chlamydia from the test material by infecting primary or continuous cell cultures, since chlamydia does not multiply on artificial nutrient media. During the cultivation process, the pathogen is identified and sensitivity to antibiotics is determined. The method of diagnostic isolation of chlamydia in cell culture can be used throughout the entire period of the disease, with the exception of the period of antibiotic therapy, and for a month after it. However, at present, this method is mainly used to monitor cure rates to identify chlamydia that are capable of carrying out a full development cycle. The sensitivity of the method ranges from 75 to 95%.
Methods for serological diagnosis of chlamydia are based on the determination of specific antibodies in the blood serum of patients or those who have had chlamydial infection. Serological tests to determine IgG in blood serum are informative in generalized forms of infection, as well as in cases where infected organs are not accessible for direct examination (for example, pelvic organs). For localized urogenital infection, it is informative to study indicators local immunity(in cervical mucus in women, in prostate secretions and seminal plasma in men). When examining infertile couples, the IgA indicator in these media is more informative than when examining blood serum. However, IgA appears in these environments some time after the onset of the inflammatory process, and, therefore, these tests are not suitable for diagnosing acute chlamydial infection.
Indicators of local immunity (IgA in secretions) are usually comparable in significance to indicators of humoral immunity (IgG in blood serum) in women and are not statistically significantly the same in men, apparently due to the presence of a blood-testis barrier. Serological tests should not be used as a cure test because antibody titres remain quite high for several months after treatment. However, they are informative in the differential diagnosis of chlamydia. The value of this method is especially high for chronic asymptomatic forms of chlamydial infection of the pelvic organs. The sensitivity and specificity of such test systems for determining antibodies to chlamydia are at least 95%.
Nucleic acid amplification methods (DNA diagnostic methods) are based on the complementary interaction of nucleic acids, which makes it possible to identify the nucleotide sequence in the genes of the desired microorganism with almost 100% accuracy. From numerous modifications this method PCR has become widespread in clinical practice. Any material of tissue origin is suitable for diagnosing chlamydial infection using the nucleic acid amplification method. The great advantage of the method is the possibility of studying material obtained non-invasively, for example, studying the first portion of morning urine. It should be noted that this study is more informative in men than in women (it is better to use cervical samples).
Determination of chlamydia nucleic acids should not be used as a control for cure, since it is possible to determine fragments of nucleic acids of non-viable microorganisms within several months after treatment. As noted above, a culture diagnostic method should be used for this purpose. The advantage of PCR is the ability to detect wide range pathogens in one clinical sample, i.e. obtain complete information about the presence of all pathogens in the clinical sample under study (Mycoplasma genitalium, Mycoplasma hominis, Ureaplasma parvum and Ureaplasma urealyticum). At the same time, it should be remembered that the use of a molecular biological diagnostic method in itself cannot be considered a guarantee against obtaining erroneous results. High sensitivity PCR requires strict adherence to special requirements for laboratory operating hours.
Treatment of urethritis, first of all, should be etiotropic and pathogenetic. Unlike others urological diseases in the treatment of bacterial and viral urethritis, much depends on epidemiological measures to sanitize the lesion reinfection, which can lead to sexual partners if they are not treated at the same time.
For microbial forms of urethritis, etiotropic therapy is possible only with bacteriological detection of the pathogen. Viral nonspecific urethritis is treated taking into account the sensitivity of the pathogen. For candidal urethritis, therapy should be antifungal. For metabolic nonspecific urethritis, measures aimed at eliminating metabolic disorders (phosphaturia and oxaluria, uraturia, cystinuria) should be considered etiotropic. Traumatic and “tumor” urethritis can be cured by eliminating etiological factors, i.e. injuries and tumors.
Pathogenetic treatment of urethritis consists of eliminating anatomical and other factors predisposing to the development of this disease. Among them are strictures of the urethra, purulent diseases individual paraurethral glands located in the submucosal layer of the urethra and in the valvulae fossae navicularis in the hanging part of the urethra in men, in women - damage to the paraurethral ducts and large glands vestibule of the vagina. Measures aimed at increasing the immunoreactivity of the body, which can be general and specific, should also be considered pathogenetic.
Therapy for nonspecific urethritis should be general and local. The use of a particular type of treatment largely depends on the phase and stage of the disease. In the acute phase should predominate or be the only general methods therapy; in the chronic phase of the disease, local treatment can be added.
Treatment of nonspecific urethritis is divided into:
Antibacterial therapy for bacterial urethritis should be carried out taking into account the sensitivity of the isolated microorganism, giving preference to semi-synthetic penicillins and cephalosporins for coccal flora, and to aminoglycosides and fluoroquinolones for non-negative flora. Some tropism of tetracyclines and macrolides towards the male genital organs should be taken into account. When selecting drugs for the treatment of nonspecific urethritis, it is necessary to take into account the capabilities of nitrofurans, especially furazolidone. They are also quite active against protozoa, Trichomonas. The greatest difficulties arise in the treatment of staphylococcal urethritis, when there are strains of bacteria that are resistant to all antibiotics and chemotherapy drugs. Such patients are indicated for treatment with staphylococcal toxoid, staphylococcal γ-globulin (human anti-staphylococcal immunoglobulin), administered intramuscularly, and if it is ineffective, an autovaccine should be obtained and administered twice.
With Reiter's syndrome, when joint damage is so pronounced. which lead to the development of ankylosis, glucocorticoid therapy is indicated. Drugs that improve microcirculation (dipyridamole), NSAIDs (indomethacin, diclofenac, etc.) are also prescribed.
Antibacterial treatment for chronic forms of urethritis should be supplemented with methods of nonspecific immunotherapy.
It is possible to prescribe pyrogenal, and since all patients with urethritis are usually treated on an outpatient basis, its daily administration is possible in a day hospital in a clinic. Instead of pyrogenal, prodigiosan can be used intramuscularly.
Nonspecific immunological treatment of chronic urethritis can be supplemented by the administration of prostate extract (prostatilen) 5 mg, diluted in 2 ml of sterile isotonic sodium chloride solution or 0.25% procaine solution intramuscularly 1 time per day, a course of 10 injections, with possible repetition after 2- 3 months
In the chronic phase of urethritis and, less often, in the subacute phase, local treatment of urethritis is sometimes indicated. When introducing medicinal substances into the urethra, it must be remembered that due to the good vascularization of the submucosal layer, its mucous membrane has significant absorption capacity. The urethra is washed with solutions of nitrofural (furatsilin) 1:5000. mercury oxycyanide 1:5000, silver nitrate 1:10000, protargol 1:2000. Recently, instillations into the urethra and its rinsing began to be carried out with a 1% solution of dioxidine or miramistin, as well as hydrocortisone 25-50 mg in glycerin or vaseline oil. However, the attitude towards local treatment should be restrained.
It is advisable to carry out combined treatment of urethritis, which should include physiotherapeutic methods (ultrahigh-frequency exposure, diathermy, electrophoresis of antibiotics, hot baths, etc.). Physiotherapy is especially indicated for complications (prostatitis, epididymitis). When treating nonspecific urethritis, sexual intercourse, consumption of alcoholic beverages, spices, and hot seasonings are prohibited.
Hospitalization of patients with urethritis is indicated when complications develop (acute urinary retention, acute prostatitis, epididymitis, epididymorchitis, acute cystitis and etc.).
Urethritis is an inflammatory process that is located in the urethra. This disease is very common, and the pathology develops regardless of the age and gender of the patient. In order to clearly understand what urethritis is in a man, what are the symptoms and methods of treating this pathology, it is necessary to clearly understand the anatomy of the male urethra.
Anatomical features and structure of the male urethra
The outlet of the bladder is the beginning of the urinary canal, which in medical and scientific circles is commonly called the urethra. This is a small-diameter reproductive tube, which has a length of 16 to 24 centimeters. It is worth noting that the female urethra is only 4 centimeters long. Exactly like this comparative characteristics and are the main reason for differences in the manifestations of urethritis in representatives of different sexes, respectively, if in women urethritis can pass without visible pathological symptoms, then in males the disease has very intense symptoms and can manifest itself soon after direct infection and the development of the inflammatory process.
The male urinary canal consists of the following sections:
prostatic department. This is part of the urethra, which is located in the prostate gland and is about 4 centimeters long. The prostatic section is also called prostate;
membranous section. Also called membranous. Its length is 2 centimeters. The beginning of the department is behind prostate gland, and ends at the base of the penis. This space of the male urethra is the narrowest;
spongy section, or spongy. It is the longest section of the urinary canal and is located inside the shaft of the penis. Compared to the membranous and prostatic, the spongy section is characterized by mobility. This section of the urethra ends with an outlet called the meatus.
The clinical picture and methods of therapy depend on the type of infectious agent that caused inflammation, the stage of neglect and intensity of the disease, the presence concomitant diseases and provoking factors. That is why the prescription of effective and adequate treatment depends on the nature of the pathology.
|
Classification of urethritis according to etiological indicators |
|
|
Non-infectious urethritis |
Infectious urethritis |
|
To diseases non-infectious nature relate: congestive urethritis - may appear due to venous stagnation in the pelvis; traumatic urethritis - appears against the background of ruptures and tears of the urethra, as well as after surgical interventions(catheterization, cystoscopy); allergic urethritis - develops due to exposure to allergens. |
Each type of infectious urethritis has its own certain type pathogen, and only with mixed urethritis can inflammation occur against the background of the action of two or more pathogenic organisms: tuberculosis; mixed; gardnerella; chlamydial; ureaplasmic; mycotic; bacterial; trichomonas; viral; mycoplasma; Trichomonas. |
|
Classification according to severity of symptoms |
Classification according to the characteristics of the disease |
|
Chronic urethritis is divided into periods without exacerbations and the acute stage: low-active urethritis; moderate degree of disease activity (urethritis); high degree of inflammation of the urinary canal. |
Fresh urethritis is divided into: torpid; subacute; |
|
Classification by disease specificity |
Classification according to the characteristics of the onset of the disease |
|
specific – these are sexually transmitted infections (chlamydia, trichomoniasis, gonorrhea) and tuberculosis; nonspecific - the causative agent of the infection is microorganisms that are constantly present in the body, but are suppressed by a healthy immune system. |
primary – the disease occurs as an isolated pathology; secondary – develops due to the presence of other diseases in the body. |

In most cases, the causative agents of urethritis are chlamydia and gonococci, while in approximately 50% of cases these infectious agents cannot be detected when examining the material.
After direct infection of the body, symptoms of urethritis appear after some time, and the time period from the moment of infection to the first signs of pathology directly depends on the incubation period of the pathogen. For allergic urethritis it is several hours, for tuberculosis - several years, for viral - several months, for candidiasis and trichomoniasis - two to three weeks, for chlamydial - 7-14 days, for gonorrheal - 3-7 days.
Most typical symptoms male urethritis are:
Availability characteristic discharge that appear from the urethra;
burning, itching and pain when urinating.

Other symptoms characteristic of STDs, such as general weakness and hyperemia, are not observed with urethritis. However, the nature of the discharge can be different and depends on the type of pathogen that caused urethritis. In most cases, green or white discharge appears with unpleasant smell, against which yellow crusts may form on the penis. The discharge is most noticeable in the morning.
In addition, along with the discharge, redness and sticking of the external opening of the urethra may be present. Pain in the lower abdomen can occur regardless of the type of urethritis, but even they are not a constant symptom of the pathology.
The process of urination is also disrupted, which initial stage quite often accompanied by cloudy urine, pain, and at the same time the number of daily urges to urinate increases. The end of this process may be accompanied by sharp pain and sometimes blood.
If the disease has become chronic, then the symptoms of the disease may disappear altogether, there will be no discharge, and the patient may only be bothered by mild itching and discomfort in the urethral area. More bright severe symptoms observed only during periods of exacerbation of the disease.
With bacterial urethritis, purulent discharge is observed, with trichomoniasis - whitish, with gonorrheal urethritis - gray-yellow or greenish. Also, the discharge may be insignificant or completely absent, but the man will be bothered by blood in the semen or urine, burning and itching during urination, swelling of the penis, and pain during sexual intercourse.

The table shows the most characteristic symptoms urethritis for its different types.
|
Non-infectious urethritis |
|
|
Traumatic urethritis |
Symptoms depend on the nature of the injury - burning and pain when urinating. |
|
Allergic urethritis |
Also pain and burning, however, a feature is the presence of allergic edema. |
|
Congestive urethritis |
Classic symptoms are often completely absent. Manifests different types sexual dysfunction. |
|
Infectious urethritis |
|
|
Tuberculous urethritis |
In most cases, it occurs against the background of renal tuberculosis or genital tuberculosis. Mycotic tuberculosis bacteria penetrate into the urethra through urine flow. Has few symptoms (sweating, increased fatigue, low-grade fever). |
|
Gardnerella urethritis |
Incubation period from one week to several months. In most cases, it is present as a component of mixed urethritis. |
|
Chlamydial urethritis |
There are no stings or burning sensations, slight discharge. In most cases it occurs chronically. |
|
Ureaplasma urethritis |
Most often accompanied by trichomoniasis or gonorrheal urethritis. The incubation period is about 1 month. There is green or white discharge, burning and itching when urinating. Symptoms worsen due to sexual intercourse or alcohol intake. |
|
Mycotic urethritis |
The incubation period is about 20 days, there is burning and itching. The discharge is watery or mucous, sometimes pale pink in color. |
|
Bacterial urethritis |
Purulent discharge. The symptoms are erased. The incubation period can last several months. |
|
Trichomonas urethritis |
It is characterized by constant itching in the area of the head of the penis, also characterized by the presence of grayish-white discharge and difficulty urinating. |
|
Viral urethritis |
The course of the pathology is sluggish, the symptoms are mild. May be accompanied by conjunctivitis or joint inflammation |
|
Mycoplasma urethritis |
Quite rarely occurs in isolation. In most cases it is combined with gonorrheal or trichomonas urethritis. |
|
Gonorrheal urethritis |
Gray-yellow discharge from the urethra, sharp pain at the time of urination. The pus contained in the urine gives it a cloudy color. Blood impurities appear in semen and urine. |

The choice of treatment for urethritis, like any other disease, is made based on diagnostic data. First of all, use the readings laboratory research. Taken into account general analysis blood and urine, urethroscopy data, examination of urethral smears, bacteriological urine culture.
Treatment procedures can be carried out on an outpatient basis; during treatment it is important to be systematic and accurate in following medical instructions; hospitalization is not necessary. If the reception antimicrobials is interrupted, carried out irregularly, or the patient drinks alcohol during therapy, the disease threatens to become chronic.
It is quite obvious that the selection of drugs for the medicinal treatment of male urethritis is carried out by a doctor, and the patient must comply with necessary rules: drink plenty of fluids, do not consume pickled, smoked foods, spices, herbs, avoid alcohol, observe personal hygiene rules, exclude sexual activity.

The selection of medications is carried out purely individually. Any infectious urethritis is treated with antibiotics. The most pronounced effect is achieved when using an antibacterial drug selected on the basis of a sensitivity test. It is thanks to this research that the most effective treatment can be selected.
Antibiotics of the cephalosporin group demonstrate excellent results in the treatment of gonorrheal urethritis. In addition to them, kanamycins, oletethrins, erythromycins, and tetracyclines can be prescribed. In this case, kanamycins must be used with extreme caution, since these drugs are highly toxic. Long-acting drugs - bicillin-5 and bicillin-3 - should be prescribed in short courses. In some cases, if gonorrheal urethritis is complicated by other infections, simultaneous use of several antibacterial drugs is practiced. In such cases, it is best to use the complex “Gentamicin” and “Azithromycin” (“Ecomed”, “Hemomycin”, “Azitrox”, “Azicide”, “Z-factor”, “Sumamed”).

In order to prevent the occurrence of candidiasis due to prolonged antibiotic therapy, Levorin, Fluconazole, Nystatin, Pimafucin and other antimycotic drugs are prescribed. The most important aspect of treatment is the individual selection of drugs. Quite often, men who suffer from gonorrheal urethritis ask friends to “prick” and use antibiotics uncontrollably and without consulting a doctor. Such self-medication is unacceptable, because long-term use strong anti-inflammatory drugs without a clear treatment plan and control of cure can lead to the transition of urethritis to a chronic form and the development of resistance of the pathogen to drugs.
In addition to antibiotics, the patient should take immunostimulating drugs and vitamins. To be completely sure that the body has freed itself from gonococcus and is completely cured, it is necessary to take control smears three times. Only after receiving negative results studies, we can assume that the patient is completely healthy.
Gardnerella, ureaplasma and mycoplasma urethritis
These types of urethritis are treated with the antibiotics lincosamines, fluoroquinolones, macrolides and tetracyclines. The tetracycline group, specifically doxycycline, is considered the most effective. A group of macrolides (clarithromycin) also gives excellent results. Immunostimulants are also prescribed.

For any specific urethritis, it is necessary to carry out simultaneous therapy for both sexual partners.
Trichomonas urethritis
If a man is diagnosed trichomonas urethritis, when selecting drugs, they turn to Metrogil, Trichopolum and Metronidazole. If urethritis is chronic, antibiotic therapy is added to treatment. In case of inadequate treatment, infertility may develop.
Candidal urethritis
Treatment of candidal urethritis in men requires a completely different approach. The main drugs to combat this pathology are antimycotic drugs, such as Pimafucin, Nystatin, Clotrimazole, Fluconazole. High-quality treatment of the underlying disease, which is the cause of candidal urethritis, is important.
Chlamydia urethritis
The only antibiotic that actively fights the causative agent of this infection is azithromycin. If you choose the wrong drug for chalmydia urethritis, serious complications – inflammatory diseases, epididymitis, Reiter's syndrome, infertility. If the patient has an individual intolerance to azithromycin, the following alternatives are used: doxycycline, levofloxacin, erythromycin, ofloxacin, clarithromycin. Immunostimulating drugs and vitamins should also be used in combination.
Viral urethritis
Treatment is carried out using antiviral drugs. The sooner treatment is started, the faster the recovery will occur. Among antiviral drugs, preference is given to: “Gerpevir”, “Famciclovir”, “Riboverine”, “Acyclovir”. It is not advisable to use antibiotics for this form of pathology, since they are not able to fight viruses.
Nonspecific chronic urethritis
Treatment of nonspecific chronic male urethritis is not as fast as for infectious ones. Chronic course The disease is often aggravated by concomitant pathologies, and the signs of the disease are mild or may be completely absent. Therefore, therapy for chronic urethritis should begin with taking immunostimulants. Only this approach makes it possible to activate the body’s defenses to fight infection. After receiving the result, antibiotic therapy is selected individually. Main feature Treatment of nonspecific forms of urethritis is the absence of the need to treat the sexual partner.

Non-infectious urethritis
For allergic urethritis it is necessary to use antihistamines. If urethritis is caused by stagnation of blood in the pelvic area (congestive), it is necessary to eliminate the cause of this stagnation. For traumatic urethritis, in addition to antimicrobial therapy, surgical intervention may also be required.
Antibiotics may be prescribed for:
installation of the drug through catheter administration into the urethra;
intravenous infusions in 0.2% of cases of acute urethritis;
intramuscular injections in 18%;
oral intake in 81%;
use of only one antibiotic - monotherapy 41%;
two – 41%;
three – 13%;
four antibiotics – 5% of cases.
The most popular antibiotics for acute male urethritis, which are prescribed by a doctor depending on the type of pathogen
|
Trichomonas urethritis in combination with atypical agents |
Gonococcal urethritis |
Mixed urethritis |
|||||
|
"Ornidazole" |
"Doxycycline" |
"Josamycin" |
|||||
|
"Josamycin" |
"Ciprofloxacin" |
"Ceftriaxone" |
|||||
|
"Azithromycin" |
"Metronidazole" |
"Ornidazole" |
|||||
|
"Doxycycline" |
"Azithromycin" |
"Secnidazole" |
|||||
|
"Metronidazole" |
"Ceftriaxone" |
"Fluconazole" |
|||||
|
"Doxycycline" |
|||||||
|
"Azithromycin" |
|||||||
|
Non-gonococcal urethritis, which is caused by atypical agents |
Urethritis of unknown etiology |
||||||
|
"Clarithromycin" |
"Clarithromycin" |
||||||
|
"Secnidazole" |
"Ciprofloxacin" |
||||||
|
"Josamycin" |
"Tinidazole" |
||||||
|
"Metronidazole" |
"Nimorazole" |
||||||
|
"Doxycycline" |
"Josamycin" |
||||||
|
"Ofloxacin" |
"Secnidazole" |
||||||
|
"Fluconazole" |
"Fluconazole" |
||||||
|
"Azithromycin" |
"Ceftriaxone" |
||||||
|
"Doxycycline" |
|||||||
|
"Metronidazole" |
|||||||
|
"Azithromycin" |
|||||||

In addition to the basic course of treatment with antibacterial drugs that suppress the acute symptoms of the disease, other healing methods, which relate to local and physiotherapeutic procedures.
Local procedures involve the injection of medications directly into the opening of the urethra. Urethral installations are performed using the drug hydrocortisone, Dioxidin and Mirimistin. Local treatment gives good results when used in combination with other drugs.
Physiotherapeutic treatment is used exclusively in cases of chronic urethritis; the use of these methods in acute inflammatory processes is strictly contraindicated. Magnetic therapy, laser therapy, UHF, electrophoresis may be prescribed. However, all these methods should be carried out only systematically and only under the supervision of specialists.
Causes of urethritis in men
sexually transmitted infections are the most common cause of urethritis in men who are sexually active. If sexual intercourse is performed without the use of means barrier contraception, then the probability of pathogen penetration into the urethra is very high;
urolithiasis - found much more often in men than in women. This disease causes traumatic urethritis, due to the fact that stones, moving along the genitourinary tract, actively injure the mucous membrane and lead to the attachment of pathogenic microorganisms;
any injury to the penis and heavy physical activity can cause the development of urethritis;
hypothermia is one of the most important provocateurs of exacerbations of chronic diseases (including extrapulmonary tuberculosis, viruses, infections), since in this case the protective functions of the body are significantly reduced;
a general decrease in immunity - smoking, alcohol abuse, overwork, lack of sleep, poor nutrition leads to a natural depletion of the body's defenses;
medical manipulations (bladder catheterization, smear) - carry the risk of injury to the mucous membrane of the urethra, and urethritis can develop if the necessary disinfection measures are not followed;

nutrition - an abundance of sour, spicy, salty foods leads to irritation of the mucous membranes, which contributes to the addition of infection. Lack of fluid causes rare urination and, accordingly, natural rinsing does not occur. genitourinary tract from harmful microorganisms that may accidentally enter the urethra.
Statistics say that every second man on the planet after 50 years has prostatitis. Do not think that prostatitis can directly cause urethritis. However, quite often the occurrence of prostatitis occurs against the background of active infectious diseases of the genitourinary system. Urethritis can cause the development of Reiter's syndrome, infertility, sexual dysfunction, colliculitis, balanoposthitis, orchitis, vesiculitis. In order to minimize the risk of complications of urethritis, a man should:
avoid excessive and intense physical activity;
do not get carried away with salty, spicy, fatty foods, alcohol;
empty the bladder at the first urge to urinate, try to “tolerate” less;
avoid hypothermia;
promptly treat any chronic pathologies;
lead a decent sex life, observe the rules of intimate hygiene.
Urethritis is a pathological inflammatory process of the mucous membrane of the urethra; it is one of the most common urological diseases not only in women, but also in men. High-quality, timely diagnosis is the key to successful and effective treatment, which minimizes the risk of developing dangerous complications. What tests for urethritis in women need to be taken before starting complex therapy?
The first method of diagnosing urethritis is examination. Clinical diseases can be:
Which doctor should I contact at the first symptoms of the disease? This can be not only a gynecologist, but also a urologist, dermatovenerologist. A woman must definitely see a gynecologist, who will send her a series of tests and studies. Only high-quality diagnostics makes it possible to accurately determine the causative agent of the disease and prescribe an effective course of treatment.
A general urine test is the fastest and most informative diagnostic method that allows you to establish the fact of an inflammatory process in the urethra. In this case, the laboratory technician will detect a large number of leukocytes in the urine. For the most reliable result, urine collection must be carried out in the morning, this should be the first portion after a night's sleep (before this, you should not urinate for at least 4 hours).
Bacteriological urine culture is the most accurate diagnostic method, allowing you to determine the causative agent of the disease and prescribe effective drugs. What is the essence of the technique?
The analysis is carried out in a microbiological laboratory. The urine sample is placed in nutrient medium with favorable conditions for the spread of infection. If there is an assumption that the patient has diarrhea, agar is used.
Bacteriological analysis not only confirms or denies the presence pathogenic microflora, but also shows the number of pathogenic microorganisms. This indicator is designated as CFU - colony-forming units. This assessment allows us to assess the severity and stage at which the inflammatory process is located.
How is the sensitivity of an infection to antibiotics determined? To do this, various antibacterial drugs. And if the antibiotic stops or inhibits the growth of the infection, it will be effective in treating this case in that patient.
Please note that in order for the tests to be accurate and reliable, it is necessary to collect urine correctly. The collection is carried out in a special plastic container in an amount of three to five milliliters. The material must be delivered to the laboratory within 2 hours after collection.
This technique makes it possible to determine the exact localization of the inflammatory process, when it is necessary to establish an accurate diagnosis and implement differential diagnosis between cystitis, urethritis and pyelonephritis.
 Timely diagnosis is the key successful treatment urethritis.
Timely diagnosis is the key successful treatment urethritis. How is the research conducted? Before the test, you should not urinate for 3-5 hours. Urine collection is carried out in the morning. The patient needs to collect urine in 3 containers (the first - 1/5 of the total volume, the second - 3/5, the third - 1/5). The material is sent to the laboratory, where a general urine test and a test using the Nechiporenko method are performed. The content of leukocytes in each portion of the material is assessed.
The results of the study are assessed as follows:
Urethral smear is reliable and exact method diagnostics, since a sample of material for analysis is taken directly from the area affected by the infection. There are several types of smears:
The material is collected using a special sterile spoon or probe. The material is placed in a special container and transferred to the laboratory. TO this study a woman should prepare:
If, during the examination, the doctor saw that pus and mucus were being released from the urethra, the discharge can be used for analysis. In this case, the study is carried out in the same way as with smears.
Often when diagnosing urethritis, it is carried out PCR analysis– an effective method for determining a large number of pathogens of infectious urethritis. The technique is often used in diagnosis inflammatory processes in the urethra, provoked by herpes viruses or chlamydia. A swab or urine sample is used as the material. Polymerase testing is carried out in the laboratory chain reaction(PCR), as a result of which the DNA of the pathogen is increased.
Urethroscopy is a study that involves inserting special equipment into the urethra to examine the mucous membrane of the urethra. Preparation for ureteroscopy is carried out in several stages:
 The smear is taken using a special spoon or “brush”
The smear is taken using a special spoon or “brush” Urethroscopy allows:
When diagnosing urethritis, the specialist may also refer the patient for additional studies:
Sources:
Lopatkin N.A.: “Guide to Urology”, 1998.