The term laparoscopy refers to endoscopic surgery carried out using miniature instruments through incisions up to 20 mm long. Nowadays this is the most popular type of surgical intervention due to its low invasiveness and minimization of postoperative complications. Unlike abdominal surgery methods, which have been practiced by doctors for more than a century, laparoscopy was first performed by a French surgeon in 1987.
Laparotomy is an abdominal operation in which an incision is made in the abdomen and the gallbladder (GB) is removed. Laparoscopy involves resection of the gallbladder through small incisions using several instruments:
- laparoscope - an optical thin tube with a miniature video camera synchronized with a computer. The operation begins with the introduction of this device into the abdominal cavity;
- insufflator - a device for supplying carbon dioxide into the abdominal cavity, “spreading apart” the internal organs and improving visibility;
- trocar - a hollow tube with a sharp stylet, with the help of which punctures are made on the abdominal wall;
- aspirator - a device for removing excess fluids from the abdominal cavity and washing it;
- endoscopic instruments are various scissors, clamps, forceps and other devices necessary for performing a specific type of laparoscopy.

Before laparoscopy of the gallbladder, the patient is given intravenous or endotracheal anesthesia with mandatory artificial ventilation.
Surgeons were very skeptical about the first “micro-operations,” but it was soon shown in practice that laparoscopy is more preferable for patients due to the minimal number of postoperative complications. However, such an operation is more difficult to perform, so it has its pros and cons relative to laparotomy.
| Parameter | Laparoscopy | Laparotomy |
|---|
| Benefits of laparoscopy
|
| Incision | 3–4 cuts of 5–20 mm | 1 cut 150–200 mm long |
| Blood loss during surgery | 30–40 ml | big |
| Pain after surgery | + (simple painkillers are enough) | +++ (need narcotic anabolic steroids) |
| Need to remove sutures | No | 7 days after surgery |
| Cosmetic defect | No | ++
|
| Risk of incisional hernia | minimal | ++
|
| Length of hospital stay | up to 2 days | 2 weeks |
| Disability | up to 3 weeks | up to 8 weeks |
| Return to physical activity | in 4–5 weeks | in 8–10 weeks |
| Motor mode after surgery | you can get up and walk on the 2nd day | you can get up and walk on the 4th day |
| Full recovery | in 3–4 months | in 5–6 months |
| Disadvantages of laparoscopy
|
| Indications | cholecystitis, cholelithiasis | cholecystitis, cholelithiasis, tumor processes |
| Contraindications | There is | minimal |
| Tool Requirements | specific | ordinary |
| Surgeon's qualifications | +++
| ++
|
| Equality of operations
|
| Preparing for surgery | regular |
| Duration of operations | 30–80 minutes |
| Anesthesia | general anesthesia |
| Complication statistics | 1–5%
|
The number of pluses in the table determines the degree of manifestation of a particular parameter, for example, severity pain after operation.
The patient tolerates laparoscopy of the gallbladder much easier than abdominal surgery. He experiences less pain, does not need narcotics and recovers faster. However, not every surgeon is able to perform it, and not all hospitals have necessary equipment. Therefore, the main disadvantage remains the high cost of laparoscopy. In addition, through small incisions it is impossible to remove large polyps and tumors that can form in the gallbladder, which explains the smaller list of indications compared to laparotomy.
Types of laparoscopy of the gastrointestinal tract
Laparoscopy on gallbladder can be carried out for several purposes. The low invasiveness of the operation allows it to be used as a diagnostic tool when, after a general examination, there are still doubtful points. In some cases, during diagnostic laparoscopy, the surgeon decides to immediately perform a therapeutic operation, for example, resection of the gallbladder.

| Type of laparoscopy | The essence of the operation | Indications |
|---|
| Cholecystectomy | gallbladder removal | - acute, calculous, chronic cholecystitis;
- polyposis
|
| Choledochotomy | disclosure common duct without affecting the gastrointestinal tract | - blockage of the duct with stones or worms;
- narrowing of the duct.
|
| Anastomosis | “connection” of the bile ducts with other organs of the gastrointestinal tract | - poor flow of bile;
- congenital anomaly of the bile ducts.
|
| Diagnostic | one incision for camera insertion and visualization of the gastrointestinal tract | unclear diagnostic picture |
In fact, these operations are not much different, so the list of contraindications for their implementation is the same. Absolute diseases include such diseases as heart attack, stroke, clotting factor disorder, obesity of the third and fourth degree, and gallbladder cancer. In the latter case, diagnostic laparoscopy can be performed, but the organ cannot be removed. Sometimes it is more expedient and safer to perform a laparotomy, for example, with peritonitis, when inflammation covers a large volume of the abdominal cavity.
TO relative contraindications include acute inflammatory processes(cholecystitis, ulcer, gastritis, pancreatitis, etc.). In case of jaundice, surgery should also not be performed, since it is a sign of the acute phase of liver pathology. The decision on the need for surgery is made based on the individual characteristics of the patient’s medical history.
Preparing for surgery
In 90% of cases, resection is performed as planned. Therefore, it is possible to carry out the following preparation for laparoscopy of the gallbladder:
- taking tests for general and biochemical studies, as well as cardiograms and coagulograms - 2 weeks before surgery;
- discontinuation of medications that reduce blood clotting (aspirin, paracetamol, diclofenac, etc.) - 7 days in advance;
- giving up alcohol, fatty and heavy foods - 3 days before;
- dry fasting (even water is prohibited) - 12 hours;
- carrying out cleansing enemas - 12 hours in advance.
Laparoscopic resection of the gallbladder
Each surgeon himself chooses how it is more convenient for him to work with the patient during laparoscopic resection of the gallbladder. In France, surgeons place the patient on a table so that the doctor can stand between his legs (French method). American doctors prefer to be located at left side from the patient (American method). In any case, to remove the gallbladder, you need to make 3–5 punctures:
- in the peri-umbilical region - a laparoscope and insufflator are inserted through this incision;
- under the sternum in the middle;
- 4–5 cm below the extreme right rib - the puncture is made at the mental intersection with the vertical running in the middle of the right collarbone;
- at the intersection of the vertical going to the edge of the right armpit and the horizontal at the level of the navel;
- the fifth incision is made only if the patient has an enlarged liver and it is difficult to view the liver with a camera.
Methods for carrying out such an operation are constantly being improved. Already, some surgeons perform gallbladder resection using three miniature incisions. As a result, tiny scars remain on the patient's body, which can only be seen through a magnifying glass.
The cost of laparoscopic resection of the gallbladder varies from 300 to 2000 dollars, depending on the clinic and the qualifications of the surgeon.
When does laparoscopy become laparotomy?

Removing the gallbladder through small incisions usually takes about 30 minutes, but in some cases the surgeon decides to stop laparoscopy and perform open abdominal surgery. The reasons for this may be:
- damage to internal organs or blood vessels with associated bleeding;
- severe inflammation and swelling of internal organs, making it difficult to visualize the surgeon’s “working area”;
- high risk of developing peritonitis;
- purulent destruction of the gallbladder wall;
- fistulas and multiple adhesions in the biliary system.
Perforation of the gastrointestinal tract (stomach, duodenum, large intestine), as well as any internal damage accompanied by bleeding is an indication for urgent laparotomy due to the risk of large blood loss. This is necessary to prevent bile leakage into the abdominal cavity and prevent peritonitis.
Possible complications
After laparoscopic resection, most patients experience mild, moderate pain in the puncture area, which can be relieved with analgesics. After a week, any discomfort will disappear and the recovery period will begin, although physical activity will have to wait for now. People who suffer from constipation are advised to use a laxative to avoid straining the muscles during bowel movements and to avoid damaging the internal sutures.

It is officially believed that the probability of postoperative complications after laparoscopic cholecystectomy is the same as during abdominal resection and is 1–5%. However, in reality, only 1 in 5,000 patients develop the following complications:
- internal bleeding as a result of vascular damage;
- “leakage” of bile in the liver and abdominal cavity;
- suppuration of internal wounds and, as a consequence, the formation of a subcutaneous abscess;
- accumulation of gas under the skin due to an incorrect puncture - this complication is more often observed in obese people, and it is not dangerous, since the “gas tubercle” soon resolves;
- spread of cancer cells into the abdominal cavity, if any were present in the biliary system.
0.5–0.7% of patients develop umbilical hernia. Obese people and those who underwent urgent surgery are most at risk for this complication.
Meanwhile, 5–30% of people who have undergone resection develop the so-called postcholecystectomy syndrome, regardless of the type of surgery - laparoscopic or open. This syndrome refers to a condition when, after resection, the patient does not feel any changes or feels worse.
Only 10% of such people are diagnosed psychological problem due to personal fear of any surgery. In 20%, the deterioration of the condition is associated with surgeon errors. For example, a piece of gallbladder tissue remains in the human body, which is an excellent source of secondary inflammation. Or, as a result of a puncture of the trocar, the bile duct was damaged, which subsequently began to narrow. In the remaining 70% of people, postcholecystectomy syndrome is caused by activation of a previously undiagnosed disease of the digestive system: pancreatitis, cholangitis, tumors, etc.
Removal of stones while preserving the gallbladder

Preserving the organ is called cholecystolithotomy. This operation cannot be called very specific, but it has its own nuances and is carried out in accordance with the following stages:
- the first incision is made, a laparoscope is inserted and a review of the condition of the gallbladder, surrounding tissues and organs is carried out;
- the following incision is made for laparotomy access, most often transrectal;
- a puncture is made in the abdominal cavity to prevent gas from escaping;
- under the control of a laparoscope, the peritoneum is dissected, and the bottom of the gallbladder is pulled towards the wound;
- The gallbladder is sutured to the wound with two threads and opened;
- by tamponing, the bleeding is stopped, and bile is removed from the gallbladder using an aspirator;
- Using a clamp and special forceps, the surgeon grabs one stone at a time and removes it from the gallbladder; the procedure is repeated until all stones are removed;
- cholecystocholangiography is performed to examine the biliary tract for damage;
- pneumocholecystoscopy is performed to examine the gallbladder cavity and confirm the absence of stones;
- the gastric wounds are sutured and abdominal wall.
This type of operation for a long time was used to treat gallstone disease, but studies have shown that it is ineffective. Firstly, the operation is more difficult, and secondly, in 2 out of 3 people who undergo it, re-formation of stones in the gallbladder occurs. Therefore, most surgeons are of the opinion that organ resection is more effective means in the treatment of cholelithiasis.
The high risk of relapse of cholelithiasis and the development of postoperative peritonitis are the main reasons why cholecystolithotomy is now rarely performed.
However, some surgeons still take on this type of work; in particular, this type of operation is still practiced in Ukraine. But the “second wind” of cholecystolithotomy was discovered by the Chinese doctor Chao Te, who has a huge number of regalia in the field of healthcare in the PRC. He now works in a clinic and research center in Guangzhou, and is also the founder of the CHIAO endoscope brand.
It should be noted that many intermediary companies are now actively using the name Chao Te to sell “medical tours”. In particular, a package is offered that includes meeting the patient at the airport, conducting all preliminary diagnostic examinations and the operation itself by Dr. Chao Te. All this will cost 36,000 yuan, which is approximately $5,000, plus round-trip airfare.
Considering that most European surgeons have long abandoned performing cholecystolithotomy, having clinically proven its ineffectiveness, it is not advisable to pay such huge amounts of money. Although each patient himself chooses what is best for him - or to clean it with a high risk of recurrence of cholelithiasis.
Gallstone disease has become one of the most common phenomena among abdominal pathologies today, and surgery to remove gallstones is one of the methods to radically solve the problem.
Gallstone disease - what is it?
This is a disease associated with the formation of stones (calculi) in the bile ducts and gallbladder. It develops for the following reasons:
- stagnation or change in the composition of bile;
- inflammatory processes;
- violation of biliary excretion (dyskinesia).
There are three types of stones based on their composition. The most common (in 80-90% of cases) are cholesterol stones. Their formation is facilitated by excess cholesterol content in bile. In this case, crystals form due to the precipitation of excess cholesterol. If the motility of the gallbladder is impaired, then these formations are not removed into the intestinal space, but remain inside it and begin to increase.
Pigment stones are formed due to increased breakdown of blood cells - red blood cells. Most often this can be observed when hemolytic anemia. There are also mixed formations. They are a combination of both forms. They contain cholesterol, bilirubin and calcium.
Is surgery necessary?
Anyone who has been diagnosed with gallstones sooner or later faces the question of whether surgical intervention is necessary or will be sufficient conservative treatment. It is worth mentioning that stones themselves are not a reason to remove the gallbladder. If they do not manifest themselves in any way and do not affect the normal functioning of other organs, then you don’t have to think about surgery. However, if there is pain in the gallbladder, a disturbance in the general condition, or jaundice, then it is necessary to urgently consult a surgeon. After the examination, it is he who will decide whether surgical intervention is necessary and what kind of intervention. But it must be taken into account that cholecystitis of the gallbladder implies an inflammatory process that has already begun. If you delay the decision excessively, then the chances of fully recovering health after surgery are sharply reduced. Even if there was a one-time attack, it is better to remove the gallstones.

Indications for surgery
When deciding whether surgery is necessary, specialists usually take into account the following factors:
- the presence of stones (concretions) of various sizes, occupying more than a third of the volume of the gallbladder;
- if the disease occurs with frequent attacks of pain in the gallbladder (biliary colic), then the operation is performed regardless of the size of the stones;
- if the stones are located both in the gallbladder and in the ducts;
- when the ability of the gallbladder to contract decreases or it completely shuts down;
- with the development of biliary pancreatitis;
- when the integrity of the walls of the gallbladder is violated;
- when the common hepatic duct is blocked.
There are international recommendations for determining the need for surgical intervention for gallstone disease. By summing up the points that are assigned to different diagnostic indicators, the doctor determines whether surgery is required, as well as the relative and absolute indications for it.
Types of operations

Typically, the process of education gallstones- it's not a quick thing. Of course, if you are unlucky and an ambulance takes you to a surgical hospital with an acute attack, which was diagnosed as cholecystitis of the gallbladder, then you have little choice. But in most cases, people who know about their problem discuss all the details in advance with the attending physician and determine the date of the planned surgical intervention.
IN modern medicine There are two methods for removing the gallbladder (cholecystectomy):
- open cholecystectomy is a traditional method that involves opening the abdominal cavity;
- Laparoscopic cholecystectomy is a more modern technique that is preferred today.
Open cholecystectomy
This operation to remove gallstones is a classic surgical procedure. Through a wide incision along the midline of the abdomen, the abdominal cavity is examined, the gallbladder is removed and, if necessary, drainage is performed (tubes are installed to ensure the outflow of the resulting exudate and other biological fluids).
Despite the emergence of more modern and high-tech methods, open cholecystectomy continues to remain relevant. This can be explained by the fact that some clinics do not have the equipment or specialists with the necessary qualifications to perform laparoscopic operations. In addition, there are certain contraindications for them.

Laparoscopy of the gallbladder
This is another type of surgery for gallstone disease. Today, this method is becoming more and more widespread due to its effectiveness, low trauma, and reduced recovery time. The operation is performed using a laparoscope - a special device that allows access to the damaged organ through several punctures in the abdominal wall, through which manipulators and, in fact, the laparoscope are inserted. This method allows not only to remove the gallbladder without leaving postoperative scars, but in some cases to remove only the stones, leaving the organ in place. Similar method used not only for the treatment of cholelithiasis, but also for the removal of appendicitis, treatment inguinal hernias, some gynecological diseases, as well as diagnostic operations. Despite the obvious advantages of laparoscopic cholecystectomy, this method has its contraindications. These include:
- an abscess located in the surgical area;
- last three months of pregnancy;
- severe cardiopulmonary pathologies.
In addition, it must be taken into account that when performing a laparoscopic operation, in case of the slightest difficulty in its course, surgeons proceed to open cholecystectomy. Approximately 5% of laparoscopic operations end this way.

Preparing for surgery
Like any surgical procedure, surgery to remove gallstones requires certain preparation. In addition to the standard examination, which includes tests (general blood count and urine test, blood biochemistry, coagulogram - blood clotting test, liver tests), it is necessary to do an ultrasound of the abdominal cavity, ECG, chest X-ray, according to FGS indications and colonoscopy, as well as get a therapist's opinion. In addition, preparation for elective surgery includes the abolition of drugs that affect blood clotting. These include various anticoagulants, vitamin E, and nonsteroidal anti-inflammatory drugs. A few days before surgery special attention requires a diet for gallstone disease. The menu should not contain heavy dishes, and starting from midnight on the day of the operation, food and drink should be completely excluded. The day before, in the morning and evening, cleansing enemas are done or special medications are taken. In the morning, take a shower using antibacterial soap.
Postoperative period
Today it is difficult to surprise anyone with cholecystectomy. This operation to remove gallstones has long been routine, and is done about as often as an appendectomy. The patient is already four hours after completion of the operation, during which he must not drink or perform sudden movements, you are allowed to turn in bed. Then you can start drinking still water in small portions (1-2 sips, but not more than 500 ml). Six hours after laparoscopic surgery, the patient can get up. It is better to do this if one of the medical personnel or relatives is nearby, since after the body has been in a horizontal position for a long time and in a state of anesthesia, dizziness and fainting may occur when trying to get up. Already on the next day after the operation, the patient can move freely around the hospital.

After surgery, diet for gallstone disease is of great importance. The menu for the next day may include liquid food - oatmeal with water, dietary soups, fermented milk products. In the future, you can include in your diet boiled beef, chicken breast, baked apples or bananas. It must be remembered that in the first week after the operation, alcohol, coffee, sugar, fried and fatty foods are prohibited.
Litholytic therapy
If surgical intervention is impossible due to severe somatic diseases or bleeding disorders, as well as if the patient refuses surgery, litholytic therapy is performed. This is a method that uses drugs containing substances designed to dissolve formed stones. When starting it, you need to take into account that the duration of treatment can be from one to two years, and even if it is possible to completely dissolve the stones in the gall bladder, this does not guarantee that they will not appear again. In addition, during the treatment process, various complications of cholelithiasis may arise, including those that require surgical intervention.
Criteria for litholytic therapy

Another limitation of litholytic therapy is certain requirements for the criteria of the disease:
- Gallstones must be cholesterol and not exceed 20 mm in size.
- preserved, and the stones do not occupy more than half of its volume.
- The cystic and common bile ducts must maintain their patency.
- Less than two years have passed since the stones formed.
- The history should include an uncomplicated course of the disease - moderate pain, rare attacks of hepatic colic.
Treatment is carried out under ultrasound control once every 3-6 months. If after six months there is no improvement, then it is considered ineffective, and the question of surgical intervention is raised again. If litholytic therapy was successful, then in order to timely detect newly formed stones in the gall bladder, ultrasound is performed at least once every three months.
To date there is not one conservative method treatment that would 100% help get rid of stones in the bile ducts (choledocholithiasis). The most effective way The treatment for cholecystitis is surgery to remove the gallbladder (cholecystectomy). In modern clinics, it is carried out in the most gentle way possible using laparoscopy after just 2-4 punctures on the body. A few hours after the procedure, the patient can already get up, and after a few days be discharged home.
Causes of gallstone disease
The gallbladder is a small organ shaped like a pouch. Its main function is the production of bile (an aggressive fluid necessary for normal digestion). Stagnation leads to the fact that individual components of bile precipitate, from which stones are subsequently formed. There are several reasons for this:
- Eating disorders. Abuse of foods high in cholesterol, fatty or salty foods, long-term consumption of highly mineralized water leads to metabolic disorders and the formation of stones in the bile ducts.
- Taking certain types of medications, especially hormonal contraceptives, increases the risk of developing calculous (inflammation of the bladder with stone formation) cholecystitis.
- Sedentary lifestyle, obesity, long-term compliance low calorie diets lead to digestive dysfunction and congestion in the biliary tract.
- The anatomical features of the structure of the gallbladder (the presence of bends or kinks) prevent the normal removal of bile and can also provoke calculous cholecystitis.
Why are stones dangerous?
As long as the stones are in the cavity of the gallbladder, a person may not even be aware of their presence. As soon as the accumulations begin to move along the bile ducts, a person is overcome by attacks of biliary colic, lasting from several minutes to 8-10 hours, dyspeptic disorders appear (difficult and painful digestion, accompanied by pain in the epigastric region, a feeling of fullness of the stomach, nausea and vomiting, heaviness in the stomach). right hypochondrium).
Choledocholithiasis (stones in the bile duct) is dangerous due to possible development inflammation of the ducts, pancreatitis, obstructive jaundice. Often, large accumulations of stones during movement become the cause of other dangerous complications:
- perforation – rupture of the gallbladder or ducts;
- peritonitis - inflammation of the peritoneum resulting from the effusion of bile into its cavity.
Long-term stagnation of bile can lead to the appearance of polyps on the walls of the organ and their malignancy (malignancy). Acute cholecystitis with the presence of stones is the reason for urgent hospitalization and prescribing surgical treatment, but even the asymptomatic course of the pathology does not exclude the possibility of performing surgery if the following indications are present:
- risk of developing hemolytic anemia;
- sedentary lifestyle life, to exclude bedsores in bedridden patients;
- jaundice;
- cholangitis - inflammation of the intrahepatic or bile ducts;
- cholesterosis – metabolic disorder and accumulation of cholesterol on the walls of the gallbladder;
- calcification – accumulation of calcium salts on the walls of an organ.
Indications for gallbladder removal
Initially, the stones formed in the bowels of the gallbladder are small in size: from 0.1 to 0.3 mm. They may go away on their own with physical therapy or medication. If these methods are ineffective, the size of the stones increases over time (some stones can reach 5 cm in diameter). They are no longer able to painlessly pass through the bile ducts, so doctors prefer to resort to removing the organ. Other indications for prescribing the procedure are:
- the presence of sharp stones that increase the risk of perforation of the organ or its parts;
- obstructive jaundice;
- acute clinical symptoms - severe pain, fever, diarrhea, vomiting;
- narrowing of the bile ducts;
- anomalies anatomical structure organ;
- patient's wishes.
Contraindications
There are general and local contraindications to cholecystectomy. If emergency surgical intervention is necessary due to a threat to human life, some of them are considered relative and may not be taken into account by the surgeon, since the benefits of treatment outweigh the possible risks. TO general contraindications relate:
- acute myocardial infarction - damage to the heart muscle caused by circulatory disorders due to thrombosis (blockage) of one of the arteries;
- stroke - acute disorder cerebral circulation;
- hemophilia – a blood clotting disorder;
- peritonitis – inflammation of a large area of the abdominal cavity;
- obesity 3 and 4 degrees;
- presence of a pacemaker;
- gallbladder cancer;
- malignant tumors on other organs;
- other diseases of internal organs in the stage of decompensation;
- late pregnancy.
Local contraindications are relative and may not be taken into account under certain circumstances. Such restrictions include:
- inflammation of the bile duct;
- peptic ulcer of the duodenum or stomach;
- cirrhosis of the liver;
- gallbladder atrophy;
- acute pancreatitis - inflammation of the pancreas;
- jaundice;
- adhesive disease;
- calcification of organ walls;
- large hernia;
- pregnancy (1st and 2nd trimester);
- abscess in the biliary tract;
- acute gangrenous or perforated cholecystitis;
- history of surgical intervention on the abdominal organs, performed via laparotomy.
Types of surgical intervention and their features
Cholecystectomy can be performed classically (using a scalpel) or using minimally invasive techniques. The choice of method depends on the patient’s condition, the nature of the pathology, and the equipment of the medical center. Each method has its own advantages and disadvantages:
- Cavity or open surgery to remove the gallbladder - midline laparotomy (an incision in the anterior abdominal wall) or oblique incisions under the costal arch. This type of surgical intervention is indicated for acute peritonitis and complex lesions of the biliary tract. During the procedure, the surgeon has good access to the affected organ, can examine its location in detail, assess the condition, and probe the bile ducts. The downside is the risk of complications and cosmetic skin defects (scars).
- Laparoscopy is the latest surgical method, thanks to which stones are removed through 2–4 small incisions (0.5–1.5 cm each) on the abdominal wall. The procedure is the “gold standard” for the treatment of chronic cholecystitis, an acute inflammatory process. During laparoscopy, the surgeon has limited access and therefore cannot assess the condition of the internal organs. The advantages of the minimally invasive technique are:
- minimum pain in the postoperative period;
- rapid restoration of working capacity;
- reducing the risk of developing postoperative complications;
- reduction in the number of days spent in hospital;
- minimum cosmetic defects on the skin.
- Mini-access cholecystectomy is a method of single laparoendoscopic access through the navel or the area of the right hypochondrium. Such actions are carried out with a minimum number of stones and no complications. The pros and cons of cholecystectomy are completely the same as standard laparoscopy.

Preparing for surgery
Before any type of cholecystectomy is performed in the hospital, the patient is visited by a surgeon and an anesthesiologist. They tell you how the procedure will take place, about the anesthesia used, possible complications and take written consent for the treatment. It is advisable to begin preparing for the procedure before hospitalization in the gastroenterology department, checking with the doctor for recommendations on diet and lifestyle, and taking tests. This will help make the procedure easier.
Preoperative
To be sure possible contraindications To achieve better treatment results, it is important not only to properly prepare for the procedure, but also to undergo an examination. Preoperative diagnostics include:
- General, biochemical blood and urine tests are completed within 7–10 days.
- A clarifying test for blood group and Rh factor - 3-5 days before the procedure.
- Testing for syphilis, hepatitis C and B, HIV - 3 months before cholecystectomy.
- Coagulogram - tests to study the hemostasis system (blood clotting test). More often it is carried out in conjunction with general or biochemical tests.
- Ultrasound of the gallbladder, biliary tract, abdominal organs - 2 weeks before the procedure.
- Electrocardiography (ECG) – diagnosis of pathologies of the cardiovascular system. It is performed a few days or a week before cholecystectomy.
- Fluorography or radiography of the chest organs - helps to identify pathologies of the heart, lungs, and diaphragm. It is given 3–5 days before cholecystectomy.
Only those people whose test results are within normal limits are allowed to undergo cholecystectomy. If diagnostic tests reveal abnormalities, you must first undergo a course of treatment aimed at normalizing the condition. Some patients, in addition to general tests, may need consultation with specialized specialists (cardiologist, gastroenterologist, endocrinologist) and clarification of the condition of the biliary tract using ultrasound or X-ray with contrast.
Since hospitalization
After hospitalization, all patients, with the exception of those who require emergency surgery, undergo preparatory procedures. General steps include compliance with the following rules:
- The day before cholecystectomy, the patient is prescribed a light meal. The last time you can eat is no later than 19.00. On the day of the procedure, you should refuse any food or water.
- The night before, you need to take a shower, shave your belly hair if necessary, and cleansing enema.
- The day before the procedure, your doctor may prescribe mild laxatives.
- If you are taking any medications, you should check with your doctor about the need to stop them.
Anesthesia
To perform cholecystectomy, general (endotracheal) anesthesia is used. At local anesthesia It is impossible to ensure complete control over breathing, relieve pain and tissue sensitivity, and relax muscles. Preparation for endotracheal anesthesia consists of several stages:
- Before surgery, the patient is given sedatives (tranquilizers or drugs with anxiolytic effect). Thanks to the premedication stage, a person approaches surgery calmly and in a balanced state.
- Before cholecystectomy, introductory anesthesia is administered. To do this, sedatives are injected intravenously to ensure sleep before the main stage of the procedure begins.
- The third stage is provision muscle relaxation. To do this, muscle relaxants are administered intravenously - drugs that strain and promote relaxation of smooth muscles.
- At the final stage, an endotracheal tube is inserted through the larynx and its end is connected to a ventilator.
The main advantages of endotracheal anesthesia are maximum safety for the patient and control over the depth of drug-induced sleep. The possibility of waking up during surgery is reduced to zero, as well as the possibility of malfunctions in the respiratory or cardiovascular system. After recovery from anesthesia, confusion, mild dizziness, headache, nausea.

How does cholecystectomy occur?
The stages of cholecystectomy may differ slightly, depending on the chosen method of excision of the gallbladder. The choice of method remains with the doctor, who takes into account all possible risks, the patient’s condition, the size and characteristics of the stones. All surgical interventions are performed only with the written consent of the patient and under general anesthesia.
Laparoscopy
Surgeries on the abdominal organs through punctures (laparoscopy) are not considered rare or innovative today. They are recognized as the “gold standard” of surgery and are used to treat 90% of diseases. Such procedures take place in a short time and involve minimal blood loss for the patient (up to 10 times less than with conventional surgery). Laparoscopy proceeds according to the following scheme:
- The doctor completely disinfects the skin at the puncture site using special chemical reagents.
- 3–4 deep incisions about 1 cm in length are made on the anterior abdominal wall.
- Then, using a special device (laparoflator), carbon dioxide is pumped under the abdominal wall. Its task is to lift the peritoneum, maximizing the viewing area of the surgical field.
- Through other incisions, a light source and special laparoscopic devices are introduced. The optics are connected to a video camera, which transmits a detailed color image of the organ to the monitor.
- The doctor controls his actions by looking at the monitor. Using instruments, the arteries and cystic duct are cut off, then the organ itself is removed.
- A drainage is placed at the site of the excised organ, all bleeding wounds are cauterized. electric shock.
- At this stage, laparoscopy is completed. The surgeon removes all devices, sutures or tapes the puncture sites.
Abdominal surgery
Open surgery is used extremely rarely today. The indications for prescribing such a procedure are: adhesion of the organ with nearby soft tissues, peritonitis, complex lesions of the biliary tract. Abdominal surgery is carried out according to the following scheme:
- After introducing the patient into a state of medical sleep, the surgeon disinfects the surface tissues.
- A small incision about 15 cm in length is then made on the right side.
- Neighboring organs are forcibly pushed back to provide maximum access to the damaged area.
- Special clips (clamps) are placed on the arteries and cystic ducts to prevent the outflow of fluid.
- The damaged organ is separated and removed, and the organ bed is treated.
- If necessary, drainage is applied and the incision is sutured.
Mini access cholecystectomy
The development of a single laparoendoscopic access method allowed surgeons to perform operations to excise internal organs, minimizing the number of surgical approaches. This method of surgical intervention has become very popular and is actively used in modern surgery clinics. The course of the mini-access operation consists of the same steps as standard laparoscopy. The only difference is that to remove the damaged organ, the doctor makes only one puncture 3–7 cm under the right costal arch or by inserting devices through the umbilical ring.
How long does the operation take?
Cholecystectomy is not considered a complex surgical procedure that would require lengthy manipulation or the involvement of multiple surgeons. The duration of the operation and the period of hospital stay depends on the chosen method of surgical intervention:
- On average, laparoscopy takes one to two hours. The hospital stay (if no complications arise during or after the operation) is 1–4 days.
- The mini-access operation lasts from 30 minutes to one and a half hours. After surgery, the patient remains under medical supervision for another 1–2 days.
- Open cholecystectomy takes from one and a half to two hours. After the operation, the person spends at least ten days in the hospital, provided that there are no complications during or after the procedure. Full rehabilitation takes up to three months. Surgical sutures are removed after 6–8 days.

Postoperative period
If a drain was installed during the operation, it is removed the next day after the procedure. Before the stitches are removed, the skin is bandaged and treated daily. antiseptic solutions. The first few hours (from 4 to 6) after cholecystectomy you need to refrain from eating, drinking, and getting out of bed is prohibited. After a day, short walks around the ward, meals and water are allowed.
If the procedure goes without complications, discomfort is minimized and is more often associated with recovery from anesthesia. Mild nausea, dizziness, and a feeling of euphoria are possible. Pain after cholecystectomy occurs when choosing open method surgical intervention. To eliminate this unpleasant symptom, analgesics are prescribed for a course of no more than 10 days. After laparoscopy, pain in the abdominal area is quite tolerable, so most patients do not need painkillers.
Since the operation involves excision of an important organ that is directly involved in the digestion process, the patient is assigned a special treatment table No. 5 (liver). The diet must be strictly followed during the first month of rehabilitation, then the diet can be gradually expanded. For the first time after cholecystectomy, it is worth limiting physical activity and not performing exercises that require tensing the abdominal muscles.
Rehabilitation and recovery
The return to the patient’s usual lifestyle after laparoscopy occurs quickly and without complications. On full recovery the body takes from 1 to 3 months. When choosing an open cavity excision method, the rehabilitation period is prolonged and lasts about six months. Feeling good and the patient’s ability to work returns two to three weeks after treatment. Starting from this period, you must adhere to the following rules:
- For a month (at least three weeks), you must adhere to rest, maintain bed rest, combining half an hour of exercise and 2-3 hours of rest.
- Any sports training or increased physical activity is allowed no earlier than three months after open surgery and 30 days after laparoscopy. You should start with minimal loads, avoiding abdominal exercises.
- During the first three months, do not lift more than three kilograms, starting from the fourth month - no more than 5 kg.
- To speed up the healing of postoperative wounds, it is recommended to undergo a course of physiotherapeutic procedures and take vitamin preparations.
Diet therapy
On the eighth or ninth day, if the operation was successful, the patient is discharged from the hospital. At this rehabilitation stage, it is important to establish proper nutrition at home, according to treatment table No. 5. You need to eat in fractions, giving preference to dietary products. All daily food should be divided into 6-7 servings. Daily calorie content of dishes: 1600–2900 kcal. It is advisable to eat at one time so that bile is produced only during meals. The last meal should be no later than two hours before bedtime.
To dilute the concentration of bile during this period, doctors recommend drinking a lot - up to two to two and a half liters of fluid per day. This can be rosehip decoction, non-acidic sterilized juices, still mineral water. For the first few weeks, all fresh fruits and vegetables are prohibited. After two months, the diet can be gradually expanded, focusing on protein food. The preferred culinary processing of dishes is boiling, steaming, stewing without fat. All food should be at a neutral temperature (about 30–40 degrees): not too hot or cold.
What can you eat if your gallbladder has been removed?
The diet needs to be structured so that it is easier for the body to cope with incoming food. You are allowed to eat no more than 50 grams of butter or 70 grams of vegetable oil per day; it is advisable to completely exclude all other animal fats. General norm bread is 200 grams, preference should be given to products made from whole grain flour with the addition of bran. The basis of the diet after surgery to remove the gallbladder should be the following products:
- Not fatty varieties meat or fish - turkey fillet, chicken, beef, pike perch, hake, perch;
- semi-liquid porridge from any cereals - rice, buckwheat, semolina, oats;
- vegetable soups or first courses with lean chicken broth, but without frying onions and carrots;
- steamed, stewed or boiled vegetables (allowed after a month of rehabilitation);
- low-fat dairy or fermented milk products - kefir, milk, yogurt, yogurt without dyes or food additives, cottage cheese;
- non-acidic berries and fruits;
- preserves, jam, mousses, soufflés, jelly, up to 25 grams of sugar per day.

List of prohibited products
To maintain the digestive system, you should completely exclude fried foods, pickled foods, spicy or smoked foods from your diet. The following are absolutely prohibited:
- fatty meat - goose, lamb, duck, pork, lard;
- fish - salmon, salmon, mackerel, flounder, sprat, sardines, halibut, catfish;
- fatty fermented milk products;
- meat broths;
- ice cream, iced drinks, soda;
- alcohol;
- conservation;
- mushrooms;
- raw vegetables;
- sour vegetable purees;
- chocolate;
- baked goods, confectionery, baked goods;
- offal;
- spicy seasonings or sauces;
- cocoa, black coffee;
- fresh wheat and rye bread;
- sorrel, spinach, onion, garlic.
Consequences of cholecystectomy
After laparoscopic removal of an organ, some patients experience postcholecystectomy syndrome, which is associated with the periodic occurrence of unpleasant sensations such as nausea, heartburn, flatulence, and diarrhea. All symptoms are successfully relieved by diet, taking digestive enzymes in tablets and antispasmodics (if necessary to eliminate pain).
It is impossible to reliably determine whether other consequences will arise after removal of the gallbladder with stones, but the patient will definitely be informed about possible problems and give recommendations on how to eliminate them. More often occur:
- Digestive disorder. Normally, bile is produced in the liver, then enters the gallbladder, where it accumulates and becomes more concentrated. After removing the storage organ, the fluid directly enters the intestines, and its concentration is lower. If a person eats large portions, bile cannot immediately process all the food, which causes: a feeling of heaviness in the stomach, bloating, and nausea.
- Risk of relapse. The absence of a gallbladder does not guarantee that new stones will not appear again after some time. You can solve the problem by following a diet, reducing cholesterol intake, and leading an active lifestyle.
- Bacterial overgrowth in the intestines. Concentrated bile not only digests food better, but also destroys some harmful bacteria and microbes living in the duodenum. The bactericidal effect of fluid coming directly from the liver is much weaker. Hence, after removal of the bladder, many patients are bothered by frequent constipation, diarrhea, and flatulence.
- Allergy. After surgery, the digestive system undergoes a number of changes: it slows down motor function gastrointestinal tract, the composition of the flora changes. These factors may serve trigger mechanism for the development of allergic reactions to certain foods, dust, pollen. To identify the irritant, allergy tests are performed.
- Stagnation of bile. It can be eliminated using a safe procedure - duodenal intubation. A special tube is inserted through the esophagus, through which a solution is supplied that helps speed up bile excretion.
Possible complications
In most cases, surgical treatment is successful, allowing the patient to quickly recover and return to a normal lifestyle. Unforeseen situations or deterioration in health are more common with abdominal surgery, but complications after removal of the gallbladder using the laparoscopic method are not excluded. Among possible consequences highlight:
- Damage to internal organs internal bleeding when blood vessels are damaged. More often it occurs at the site of insertion of the trocar (laparoscopic manipulator) and is stopped by suturing. Sometimes bleeding is possible from the liver, then they resort to the method of electrocoagulation.
- Damage to the ducts. Leads to the fact that bile begins to accumulate in the abdominal cavity. If the damage was noticeable at the stage of laparoscopy, the surgeon continues the operation using an open method, otherwise repeated surgery will be necessary.
- Suppuration postoperative suture. The complication occurs very rarely. To stop suppuration, antibiotics and antiseptic drugs are prescribed.
- Subcutaneous emphysema (accumulation of carbon dioxide under the skin). Often occurs in obese patients due to the tube getting into the skin rather than into the abdominal cavity. The gas is removed after surgery using a needle.
- Thromboembolic complications. Occur extremely rarely and lead to thrombosis pulmonary arteries or inferior vena cava. The patient is prescribed bed rest and anticoagulants - medications that reduce blood clotting.

Drug treatment for relapses
To maintain the functionality of the gastrointestinal tract and prevent bile stagnation, drug therapy is prescribed. Treatment after gallbladder removal involves the use of the following groups medications:
- Enzymes - help break down food, improve the functioning of the digestive system, stimulate the production of pancreatic juice. As part of such medicines There are pancreatic enzymes that break down proteins, fats and carbohydrates. Enzyme preparations well tolerated and side effects(constipation, nausea, diarrhea) occur extremely rarely. Popular tablets include:
- Mezim (1 tablet with meals);
- Festal (1-2 tablets before or after meals);
- Liobil (1–3 tablets after meals);
- Enterosan (1 capsule 15 minutes before meals);
- Hepatosan (1-2 capsules 15 minutes before meals).
- Choleretic agents – protect the liver from stagnation of liver secretions, normalize digestion and intestinal function. Most of these medications are herbal based and rarely cause side effects. Popular choleretic medications include:
- Cholenzym (1 tablet 1–3 times a day);
- Cyclovalon (0.1 gram 4 times a day);
- Allochol (1-2 tablets 3-4 times a day);
- Osalmid (1-2 tablets 3 times a day).
- Litholytic medications (hepatoprotectors) – restore damaged cells liver, increase the production of bile, dilute and improve its composition. The following medications have proven themselves to be effective:
- Ursofalk (patients weighing up to 60 kg, 2 capsules per day, over 60 kg - 3 drops);
- Ursosan (10–15 mg of the drug per day).
How much does gallbladder surgery cost?
The price of the procedure depends on the equipment used, the complexity of the surgical procedures and the qualifications of the doctor. The cost of the procedure may vary depending on the region of residence of the patient. Emergency cholecystectomy is performed free of charge, regardless of the patient’s citizenship and place of residence. Approximate prices for procedures in Moscow are presented in the table:
Video
Removal of the gallbladder is considered one of the most common operations. It indicated for cholelithiasis, acute and chronic cholecystitis, polyps and neoplasms. The operation is performed open access, minimally invasive and laparoscopically.
Gallbladder - important organ digestion, which serves as a reservoir of bile necessary for digesting food. However, it often creates significant problems. The presence of stones and the inflammatory process provoke pain, discomfort in the hypochondrium, and dyspepsia. Often pain syndrome so pronounced that patients are ready to get rid of the bubble once and for all, just not to experience any more torment.
In addition to subjective symptoms, damage to this organ can cause serious complications, in particular, peritonitis, cholangitis, biliary colic, jaundice, and then there is no choice - surgery is vital.
Below we will try to figure out when you need to remove your gallbladder, how to prepare for surgery, what types of interventions are possible, and how you should change your life after treatment.
When is surgery needed?
Regardless of the type of planned intervention, be it laparoscopy or cavitary removal gallbladder, testimony for surgical treatment are:
- Cholelithiasis.
- Acute and chronic inflammation of the bladder.
- Cholesterosis with impaired bile excretion function.
- Polyposis.
- Some functional disorders.
Cholelithiasis usually appears main reason most cholecystectomies. This is due to the fact that the presence of stones in the gall bladder often causes attacks of biliary colic, which recurs in more than 70% of patients. In addition, stones contribute to the development of other dangerous complications (perforation, peritonitis).
In some cases, the disease proceeds without acute symptoms, but with heaviness in the hypochondrium, dyspeptic disorders. These patients also require surgery, which is performed as planned, and its main purpose is to prevent complications.
Gallstones can also be found in the ducts (choledocholithiasis), which is dangerous due to possible obstructive jaundice, inflammation of the ducts, and pancreatitis. The operation is always complemented by drainage of the ducts.
Asymptomatic cholelithiasis does not exclude the possibility of surgery, which becomes necessary with the development of hemolytic anemia, when the size of the stones exceeds 2.5-3 cm due to the possibility of bedsores, with high risk complications in young patients.
Cholecystitis is an inflammation of the gallbladder wall, occurring acutely or chronically, with relapses and improvements replacing each other. Acute cholecystitis with the presence of stones is a reason for urgent surgery. The chronic course of the disease allows it to be carried out plannedly, possibly laparoscopically.
Cholesterosis It is asymptomatic for a long time and can be detected by chance, and it becomes an indication for cholecystectomy when it causes symptoms of damage to the gallbladder and disruption of its function (pain, jaundice, dyspepsia). In the presence of stones, even asymptomatic cholesterosis serves as a reason to remove the organ. If calcification occurs in the gallbladder, when calcium salts are deposited in the wall, then surgery is mandatory.
Presence of polyps is fraught with malignancy, therefore removal of the gallbladder with polyps is necessary if they exceed 10 mm, have a thin stalk, or are combined with cholelithiasis.
Functional disorders biliary excretion usually serves as a reason for conservative treatment, but abroad such patients are still operated on due to pain, decreased release of bile into the intestines and dyspeptic disorders.
There are also contraindications for cholecystectomy surgery, which can be general and local. Of course, if urgent surgical treatment is necessary due to a threat to the patient’s life, some of them are considered relative, since the benefits of treatment are disproportionately higher than the possible risks.
TO general contraindications include terminal conditions, severe decompensated pathology of internal organs, metabolic disorders, which can complicate the operation, but the surgeon will “turn a blind eye” to them if the patient needs to save life.
General contraindications to laparoscopy considered diseases of internal organs in the stage of decompensation, peritonitis, long-term pregnancy, pathology of hemostasis.
Local restrictions are relative, and the possibility of laparoscopic surgery is determined by the experience and qualifications of the doctor, the availability of appropriate equipment, and the willingness of not only the surgeon, but also the patient to take a certain risk. These include adhesive disease, calcification of the gallbladder wall, acute cholecystitis, if more than three days have passed since the onset of the disease, pregnancy in the first and third trimesters, large hernias. If it is impossible to continue the operation laparoscopically, the doctor will be forced to switch to abdominal intervention.
Types and features of operations to remove the gallbladder
Gallbladder removal surgery can be performed both classically, openly, and using minimally invasive techniques (laparoscopically, from a mini-access). The choice of method determines the patient’s condition, the nature of the pathology, the doctor’s discretion and the equipment of the medical institution. All interventions require general anesthesia.
Open surgery
Cavitary removal of the gallbladder involves a midline laparotomy (access along the midline of the abdomen) or oblique incisions under the costal arch. In this case, the surgeon has good access to the gallbladder and ducts, the ability to examine, measure, probe, and examine them using contrast agents.
Open surgery is indicated for acute inflammation with peritonitis and complex lesions of the biliary tract. Among the disadvantages of cholecystectomy using this method are major surgical trauma, poor cosmetic results, and complications (disruption of the intestines and other internal organs).
The course of open surgery includes:
- An incision in the anterior abdominal wall, revision of the affected area;
- Isolation and ligation (or clipping) of the cystic duct and artery supplying blood to the gallbladder;
- Separation and extraction of the bladder, treatment of the organ bed;
- Application of drainages (as indicated), suturing of the surgical wound.
Laparoscopic cholecystectomy
Laparoscopic surgery is recognized as the “gold standard” of treatment for chronic cholecystitis and cholelithiasis, and serves as the method of choice for acute inflammatory processes. The undoubted advantage of the method is considered to be minimal surgical trauma, short term recovery, minor pain. Laparoscopy allows the patient to leave the hospital 2-3 days after treatment and quickly return to normal life.
 Stages of laparoscopic surgery include:
Stages of laparoscopic surgery include:
- Punctures of the abdominal wall through which instruments are inserted (trocars, video camera, manipulators);
- Injection of carbon dioxide into the abdomen to provide vision;
- Clipping and cutting off the cystic duct and artery;
- Removal of the gallbladder from the abdominal cavity, instruments and suturing of the holes.
The operation lasts no more than an hour, but perhaps longer (up to 2 hours) if access to the affected area is difficult, anatomical features etc. If there are stones in the gall bladder, they are crushed before removing the organ into smaller fragments. In some cases, upon completion of the operation, the surgeon installs a drainage in the subhepatic space to ensure the outflow of fluid that may form as a result of surgical trauma.
Video: laparoscopic cholecystectomy, operation progress
Mini access cholecystectomy
It is clear that most patients would prefer laparoscopic surgery, but it may be contraindicated in a number of conditions. In such a situation, specialists resort to minimally invasive techniques. Mini-access cholecystectomy is a cross between abdominal and laparoscopic surgery.
The course of the intervention includes the same stages as other types of cholecystectomy: formation of access, ligation and intersection of the duct and artery with subsequent removal of the bladder, and the difference is that To carry out these manipulations, the doctor uses a small (3-7 cm) incision under the right costal arch.
The minimal incision, on the one hand, is not accompanied big injury abdominal tissues, on the other hand, provides a sufficient overview for the surgeon to assess the condition of the organs. This operation is especially indicated for patients with a strong adhesive process, inflammatory tissue infiltration, when the introduction of carbon dioxide is difficult and, accordingly, laparoscopy is impossible.
After minimally invasive removal of the gallbladder, the patient spends 3-5 days in the hospital, that is, longer than after laparoscopy, but less than in the case of open surgery. The postoperative period is easier than after abdominal cholecystectomy, and the patient returns home earlier to his usual activities.
Every patient suffering from one or another disease of the gallbladder and ducts is most interested in exactly how the operation will be performed, wanting it to be the least traumatic. In this case, there cannot be a definite answer, because the choice depends on the nature of the disease and many other reasons. So, with peritonitis, acute inflammation and severe forms pathology, the doctor will most likely be forced to undergo the most traumatic open surgery. In case of adhesions, minimally invasive cholecystectomy is preferable, and if there are no contraindications to laparoscopy, laparoscopic technique, respectively.
Preoperative preparation
For the best treatment outcome, it is important to conduct adequate preoperative preparation and examination of the patient.

For this purpose, the following is carried out:
- General and biochemical blood and urine tests, tests for syphilis, hepatitis B and C;
- Coagulogram;
- Clarification of blood type and Rh factor;
- Ultrasound of the gallbladder, biliary tract, abdominal organs;
- X-ray (fluorography) of the lungs;
- According to indications – fibrogastroscopy, colonoscopy.
Some patients need consultation with specialized specialists (gastroenterologist, cardiologist, endocrinologist), all – with a therapist. To clarify the condition of the biliary tract, additional research using ultrasound and radiopaque techniques. Severe pathology of internal organs should be compensated as much as possible, blood pressure should be brought back to normal, and blood sugar levels should be monitored in diabetics.
Preparation for surgery from the moment of hospitalization includes eating a light meal the day before, completely refusing food and water from 6-7 pm before the operation, and in the evening and morning before the intervention the patient is given a cleansing enema. In the morning you should take a shower and change into clean clothes.
If it is necessary to perform an urgent operation, the time for examinations and preparation is much less, so the doctor is forced to limit himself to general clinical examinations and ultrasound, allocating no more than two hours for all procedures.
After operation…
The length of time you spend in the hospital depends on the type of surgery performed. With an open cholecystectomy, the sutures are removed after about a week, and the length of hospitalization is about two weeks. In the case of laparoscopy, the patient is discharged after 2-4 days. Working capacity is restored in the first case within one to two months, in the second – up to 20 days after surgery. Sick leave issued for the entire period of hospitalization and three days after discharge, then at the discretion of the clinic doctor.

The next day after surgery, the drainage, if one was installed, is removed. This procedure is painless. Before the sutures are removed, they are treated daily with antiseptic solutions.
For the first 4-6 hours after removal of the bladder, you should refrain from eating and drinking water, and do not get out of bed. After this time, you can try to get up, but be careful, since dizziness and fainting are possible after anesthesia.
Almost every patient may experience pain after surgery, but the intensity varies with different treatment approaches. Of course, one cannot expect painless healing of a large wound after open surgery, and pain in this situation is a natural component of the postoperative condition. To eliminate it, analgesics are prescribed. After laparoscopic cholecystectomy, pain is less and quite tolerable, and most patients do not require pain medications.
 A day after the operation, you are allowed to stand up, walk around the room, and take food and water. The diet after removal of the gallbladder is of particular importance. In the first few days you can eat porridge, light soups, fermented milk products, bananas, vegetable purees, and lean boiled meat. Coffee, strong tea, alcohol, confectionery, fried and spicy foods are strictly prohibited.
A day after the operation, you are allowed to stand up, walk around the room, and take food and water. The diet after removal of the gallbladder is of particular importance. In the first few days you can eat porridge, light soups, fermented milk products, bananas, vegetable purees, and lean boiled meat. Coffee, strong tea, alcohol, confectionery, fried and spicy foods are strictly prohibited.
Since after cholecystectomy the patient is deprived of an important organ that accumulates and secretes bile in a timely manner, he will have to adapt to the changed conditions of digestion. The diet after removal of the gallbladder corresponds to table No. 5 (liver). You should not eat fried and fatty foods, smoked foods and many spices that require increased secretion of digestive secretions; canned food, marinades, eggs, alcohol, coffee, sweets, fatty creams and butter are prohibited.
First month after surgery you need to stick to 5-6 meals a day, taking food in small portions, you need to drink up to one and a half liters of water per day. It is allowed to eat white bread, boiled meat and fish, porridge, jelly, fermented milk products, stewed or steamed vegetables.
In general, life after removal of the gallbladder does not have significant restrictions; 2-3 weeks after treatment you can return to your usual lifestyle and work activity. The diet is indicated in the first month, then the diet gradually expands. In principle, you can eat everything, but you should not get carried away with foods that require increased bile secretion (fatty, fried foods).
In the first month after the operation, you will need to somewhat limit physical activity, not lifting more than 2-3 kg and not performing exercises that require tensing the abdominal muscles. During this period, a scar is formed, which is why restrictions are associated.
Video: rehabilitation after cholecystectomy
Possible complications
Usually, cholecystectomy proceeds quite well, but some complications are still possible, especially in elderly patients, in the presence of severe concomitant pathology, and in complex forms of damage to the biliary tract.
Among the consequences are:
- Suppuration of the postoperative suture;
- Bleeding and abscesses in the abdomen (very rare);
- Bile leakage;
- Damage to the bile ducts during surgery;
- Allergic reactions;
- Thromboembolic complications;
- Exacerbation of another chronic pathology.
A possible consequence of open interventions is often an adhesive process, especially in common forms of inflammation, acute cholecystitis and cholangitis.
Patient reviews depend on the type of surgery they underwent. The best impression, of course, is left behind by laparoscopic cholecystectomy, when literally the day after the operation the patient feels well, is active and is preparing for discharge. A more complex postoperative period and greater trauma during classical surgery cause more serious discomfort, so this operation is scary for many.
Urgent cholecystectomy, for health reasons, is performed free of charge, regardless of the place of residence, solvency and citizenship of patients. The desire to remove the gallbladder for a fee may require some costs. The cost of laparoscopic cholecystectomy ranges on average between 50-70 thousand rubles, removing a bubble from mini-access will cost about 50 thousand in private medical centers, in public hospitals you can “keep within” 25-30 thousand, depending on the complexity of the intervention and the necessary examinations.
operaciya.info
Laparoscopy of the gallbladder - definition, general characteristics, types of operations
 The term “gallbladder laparoscopy” in everyday speech usually means an operation to remove the gallbladder, performed using a laparoscopic approach. In more rare cases, this term may mean that people are removing stones from the gallbladder using laparoscopic surgery.
The term “gallbladder laparoscopy” in everyday speech usually means an operation to remove the gallbladder, performed using a laparoscopic approach. In more rare cases, this term may mean that people are removing stones from the gallbladder using laparoscopic surgery.
That is, “laparoscopy of the gallbladder” is, first of all, a surgical operation, during which either the complete removal of the entire organ is performed, or the stones present in it are removed. Distinctive feature operation is the access through which it is performed. This access is carried out using a special device - laparoscope, and therefore is called laparoscopic. Thus, laparoscopy of the gallbladder is a surgical operation performed using a laparoscope.
In order to clearly understand and imagine what the differences are between conventional and laparoscopic surgery, it is necessary to have a general understanding of the process and essence of both techniques.
So, a usual operation on the abdominal organs, including the gall bladder, is carried out using an incision in the anterior abdominal wall, through which the doctor sees the organs with his eye and can perform various manipulations on them with instruments in his hands. That is, it is quite easy to imagine a regular operation to remove the gallbladder - the doctor cuts the stomach, cuts out the bladder and stitches the wound. After such a conventional operation, a scar always remains on the skin in the form of a scar corresponding to the line of the incision made. This scar will never allow its owner to forget about the operation performed. Since the operation is performed using an incision in the tissue of the anterior abdominal wall, such access to the internal organs is traditionally called laparotomy
.
The term "laparotomy" is formed from two words - "lapar-", which translates as belly, and "tomia", meaning to cut. That is, the general translation of the term “laparotomy” sounds like cutting the stomach. Since as a result of cutting the abdomen, the doctor is able to manipulate the gallbladder and other abdominal organs, the process of such cutting of the anterior abdominal wall is called laparotomy access. In this case, access refers to a technique that allows the doctor to perform any actions on internal organs.
Laparoscopic surgery on the abdominal and pelvic organs, including the gallbladder, is performed using special instruments - a laparoscope and trocar manipulators. A laparoscope is a video camera with a lighting device (flashlight), which is inserted into the abdominal cavity through a puncture on the anterior abdominal wall. Then the image from the video camera is shown on a screen on which the doctor sees the internal organs. It is based on this image that he will carry out the operation. That is, during laparoscopy, the doctor sees the organs not through an incision in the abdomen, but through a video camera inserted into the abdominal cavity. The puncture through which the laparoscope is inserted has a length of 1.5 to 2 cm, so a small and almost invisible scar remains in its place.
In addition to the laparoscope, two more special hollow tubes called trocars or manipulators, which are designed to control surgical instruments. Through hollow holes inside the tubes, instruments are delivered into the abdominal cavity to the organ that will be operated on. After this, using special devices on the trocars, they begin to move the instruments and perform necessary actions, for example, cutting adhesions, applying clamps, cauterizing blood vessels, etc. Controlling instruments using trocars can be roughly compared to driving a car, airplane or other device.
Thus, laparoscopic surgery involves the insertion of three tubes into the abdominal cavity through small punctures 1.5–2 cm long, one of which is intended for obtaining an image, and the other two for performing the actual surgical procedure.
The technique, course and essence of the operations that are performed using laparoscopy and laparotomy are exactly the same. This means that the removal of the gallbladder will be performed according to the same rules and steps both using laparoscopy and during laparotomy.
That is, in addition to the classic laparotomy approach, laparoscopic access can be used to perform the same operations. In this case, the operation is called laparoscopic, or simply laparoscopy. After the words “laparoscopy” and “laparoscopic”, the name of the operation performed is usually added, for example, removal, after which the organ on which the intervention was performed is indicated. For example, the correct name for removing the gallbladder during laparoscopy would be “laparoscopic removal of the gallbladder.” However, in practice, the name of the operation (removal of part or the entire organ, enucleation of stones, etc.) is skipped, as a result of which only an indication of the laparoscopic approach and the name of the organ on which the intervention was performed remains.
Two types of gall bladder interventions can be performed using laparoscopic access:
1.
Removal of the gallbladder.
2.
Removing stones from the gallbladder.
 Currently surgery to remove gallstones is almost never performed for two main reasons. Firstly, if there are a lot of stones, then the entire organ should be removed, which is already too much pathologically changed and therefore will never function normally. In this case, removing only the stones and leaving the gallbladder is unjustified, since the organ will constantly become inflamed and provoke other diseases.
Currently surgery to remove gallstones is almost never performed for two main reasons. Firstly, if there are a lot of stones, then the entire organ should be removed, which is already too much pathologically changed and therefore will never function normally. In this case, removing only the stones and leaving the gallbladder is unjustified, since the organ will constantly become inflamed and provoke other diseases.
And if there are few stones or they are small, then you can use other methods to remove them (for example, litholytic therapy with ursodeoxycholic acid preparations, such as Ursosan, Ursofalk, etc., or crushing stones with ultrasound, due to which they decrease in size and independently exit the bladder into the intestine, from where they are removed from the body along with food bolus and feces). For small stones, litholytic therapy with medications or ultrasound is also effective and avoids surgery.
In other words, the current situation is that when a person needs surgery for gallstones, it is advisable to remove the entire organ completely, rather than remove the stones. This is why surgeons most often resort to laparoscopic removal of the gallbladder, rather than stones from it.
Advantages of laparoscopy over laparotomy
 Laparoscopy has the following advantages over major abdominal surgery:
Laparoscopy has the following advantages over major abdominal surgery:
- Little damage to the tissue of the anterior abdominal wall, since the operation uses four punctures rather than an incision;
- Minor pain after surgery, subsiding within 24 hours;
- A few hours after the end of the operation, the person can walk and perform simple actions;
- Short hospital stay (1 – 4 days);
- Rapid rehabilitation and restoration of working capacity;
- Low risk of postoperative hernia;
- Subtle or almost invisible scars.
Anesthesia for laparoscopy of the gallbladder
To perform laparoscopy, only general endotracheal anesthesia is used with the mandatory connection of a ventilator. Endotracheal anesthesia is gas and formally represents a special tube through which a person will breathe using a ventilator. If endotracheal anesthesia is not possible, for example, in people suffering from bronchial asthma, intravenous anesthesia is used, which is also necessarily combined with artificial ventilation.
Laparoscopic removal of the gallbladder - the course of the operation
Laparoscopic surgery is performed under general anesthesia, just like laparotomy, since only this method allows not only to reliably relieve pain and tissue sensitivity, but also to relax the abdominal muscles well. With local anesthesia, it is impossible to provide reliable relief of pain and tissue sensitivity in combination with muscle relaxation.
After a person is put under anesthesia, the anesthesiologist inserts a tube into the stomach to remove the liquid and gases present in it. This probe is necessary to prevent accidental vomiting and the entry of stomach contents into the respiratory tract with subsequent asphyxia. The gastric tube remains in the esophagus until the end of the operation. After the tube is installed, the mouth and nose are covered with a mask attached to a ventilator, with which the person will breathe during the entire operation. Mechanical ventilation during laparoscopy is absolutely necessary, since the gas used during the operation and pumped into the abdominal cavity puts pressure on the diaphragm, which, in turn, strongly compresses the lungs, as a result of which they cannot breathe on their own.
Only after the person has been put under anesthesia, gases and fluids have been removed from the stomach, and a ventilator has been successfully attached, the surgeon and his assistants begin to perform laparoscopic surgery to remove the gallbladder. To do this, a semicircular incision is made in the navel fold, through which a trocar with a camera and a flashlight is inserted. However, before the camera and flashlight are inserted, sterile gas, most often carbon dioxide, is pumped into the abdomen, which is necessary to straighten the organs and increase the volume of the abdominal cavity. Thanks to the gas bubble, the doctor is able to freely operate trocars in the abdominal cavity, minimally affecting neighboring organs.
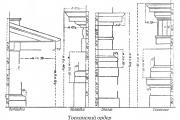
Then, along the right hypochondrium, another 2 to 3 trocars are inserted, with which the surgeon will manipulate the instruments and remove the gallbladder. The puncture points on the abdominal skin through which trocars are inserted for laparoscopic removal of the gallbladder are shown in Figure 1.

Picture 1– Points at which a puncture is made and trocars are inserted for laparoscopic removal of the gallbladder.
The surgeon then first examines the location and appearance of the gallbladder. If the bladder is closed by adhesions due to a chronic inflammatory process, then the doctor first dissects them, releasing the organ. Then the degree of its tension and fullness is determined. If the gallbladder is very tense, the doctor first cuts its wall and sucks out a small amount of fluid. Only after this a clamp is applied to the bladder, and the common bile duct, the bile duct, is released from the tissues, connecting it to the duodenum. The common bile duct is cut, after which the cystic artery is isolated from the tissue. Clamps are applied to the vessel, it is cut between them and the lumen of the artery is carefully sutured.
Only after the gallbladder is freed from the artery and common bile duct, the doctor begins to isolate it from the hepatic bed. The bubble is separated slowly and gradually, cauterizing all bleeding vessels along the way with an electric current. When the bubble is separated from the surrounding tissue, it is removed through a special small cosmetic puncture in the navel.
After this, the doctor, using a laparoscope, carefully examines the abdominal cavity for bleeding vessels, bile and other pathologically altered structures. The vessels are coagulated, and all altered tissues are removed, after which an antiseptic solution is injected into the abdominal cavity, which is used to rinse it, after which it is sucked out.
This completes the laparoscopic operation to remove the gallbladder; the doctor removes all trocars and sutures or simply seals the punctures in the skin. However, a drainage tube is sometimes inserted into one of the punctures and left for 1 to 2 days so that the remaining antiseptic lavage fluid can flow freely from the abdominal cavity. But if during the operation practically no bile was poured out, and the bladder was not very inflamed, then the drainage may not be left.
It should be remembered that laparoscopic surgery can be converted to laparotomy if the bubble is too tightly fused with the surrounding tissues and cannot be removed using the available instruments. In principle, if any unsolvable difficulties arise, the doctor removes the trocars and performs a conventional extended laparotomy operation.
Laparoscopy of gallbladder stones - the course of the operation
The rules for inducing anesthesia, installing a gastric tube, connecting a ventilator and inserting trocars to remove stones from the gallbladder are exactly the same as for cholecystectomy (removal of the gallbladder).
After introducing gas and trocars into the abdominal cavity, the doctor, if necessary, cuts off adhesions between the gallbladder and surrounding organs and tissues, if any. Then the wall of the gallbladder is cut, the tip of the suction is inserted into the cavity of the organ, with the help of which all the contents are removed out. After this, the gallbladder wall is sutured, the abdominal cavity is washed with antiseptic solutions, the trocars are removed and sutures are placed on the punctures in the skin.
Laparoscopic removal of gallstones can also be converted to laparotomy at any time if the surgeon encounters any difficulties.
How long does gallbladder laparoscopy take?
Depending on the experience of the surgeon and the complexity of the operation, laparoscopy of the gallbladder lasts from 40 minutes to 1.5 hours. On average, laparoscopic gallbladder removal takes about an hour.
Where to have the operation?
You can undergo laparoscopic surgery to remove the gallbladder in the central regional or city hospital in the general department surgery or gastroenterology. In addition, this operation can be performed in research institutes dealing with diseases of the digestive system.
Laparoscopy of the gallbladder - contraindications and indications for surgery
 Indication The following diseases require removal of the gallbladder using the laparoscopic method:
Indication The following diseases require removal of the gallbladder using the laparoscopic method:
- Chronic calculous and non-calculous cholecystitis;
- Polyps and cholesterosis of the gallbladder;
- Acute cholecystitis (in the first 2–3 days from the onset of the disease);
- Asymptomatic cholecystolithiasis (gallbladder stones).
Carrying out laparoscopic removal of the gallbladder contraindicated in the following cases:
- Abscess in the gallbladder area;
- Severe diseases of the cardiovascular or respiratory system in the stage of decompensation;
- Third trimester of pregnancy (from 27 weeks to birth);
- Unclear location of organs in the abdominal cavity;
- Operations on the abdominal organs performed in the past via laparotomy;
- Intrahepatic location of the gallbladder;
- Acute pancreatitis;
- Obstructive jaundice resulting from blockage of the bile ducts;
- Suspicion of the presence malignant tumor in the gallbladder;
- Severe scarring in the hepatic ligament or neck of the gallbladder;
- Blood clotting disorders;
- Fistulas between the biliary tract and intestines;
- Acute gangrenous or perforated cholecystitis;
- “Porcelain” cholecystitis;
- Presence of a pacemaker.
Preparation for laparoscopy of the gallbladder
The following tests should be taken a maximum of 2 weeks before the planned surgery:
- General blood and urine analysis;
- Biochemical blood test with determination of bilirubin concentration, total protein, glucose, alkaline phosphatase;
- Coagulogram (APTT, PTI, INR, TV, fibrinogen);
- Blood type and Rh factor;
- Vaginal flora smear for women;
- Blood for HIV, syphilis, hepatitis B and C;
- Electrocardiogram.
A person is allowed to undergo surgery only if the results of his tests are within normal limits. If there are deviations from the norm in the tests, you will first have to take a course necessary treatment aimed at normalizing the condition.
In addition, in the process of preparing for laparoscopy of the gallbladder, you should take control of the course of existing chronic diseases of the respiratory, digestive and endocrine systems and take medications agreed with the surgeon who will operate.
On the day before surgery, you should finish eating at 6:00 pm and drinking at 10:00 pm. From ten o'clock on the evening before surgery, a person must neither eat nor drink until the start of surgery. To cleanse the intestines on the day before surgery, you should take a laxative and give an enema. An enema should also be given in the morning immediately before surgery. Laparoscopic removal of the gallbladder does not require any other preparation. However, if in any individual case the doctor considers it necessary to perform any additional preparatory manipulations, he will say this separately.
Laparoscopy of the gallbladder - postoperative period
After the operation is completed, the anesthesiologist “wakes up” the person by stopping giving the anesthetic gas mixture. On the day of surgery, you should remain in bed for 4 to 6 hours. And after 4 to 6 hours after the operation, you can turn around in bed, sit down, stand up, walk and perform simple self-care actions. Also from this moment you are allowed to drink still water.
On the second day after surgery, you can start eating light, soft foods, for example, weak broth, fruits, low-fat cottage cheese, yogurt, boiled lean minced meat, etc. Food should be taken frequently (5 – 7 times a day), but in small portions. During the entire second day after surgery, you need to drink a lot. On the third day after surgery, you can eat regular food, avoiding foods that cause severe gas (legumes, brown bread, etc.) and bile secretion (garlic, onions, hot, salty, spicy foods). In principle, from 3 to 4 days after the operation you can eat according to diet No. 5, which will be described in detail in the corresponding section.
For 1–2 days after surgery, a person may experience pain in the area of punctures on the skin, in the right hypochondrium, and also above the collarbone. These pains are caused by traumatic tissue damage and will completely disappear in 1 to 4 days. If the pain does not subside, but, on the contrary, intensifies, you should immediately consult a doctor, as this may be a symptom of complications.
During the entire postoperative period, which lasts 7–10 days, you should not lift heavy objects or perform any work related to physical activity. Also during this period you need to wear soft underwear that will not irritate painful punctures on the skin. The postoperative period ends on days 7–10, when the sutures from the punctures on the abdomen are removed in the clinic.
Sick leave for laparoscopy of the gallbladder
A sick leave certificate is given to a person for the entire period of stay in the hospital plus another 10 to 12 days. Since discharge from the hospital occurs on days 3–7 after surgery, the total sick leave for gallbladder laparoscopy ranges from 13 to 19 days.
If any complications develop, the sick leave is extended, but in this case the period of incapacity for work is determined individually.
After laparoscopy of the gallbladder (rehabilitation, recovery and lifestyle)
 Rehabilitation after laparoscopy of the gallbladder usually proceeds quite quickly and without complications. Complete rehabilitation, including both physical and mental aspects, occurs 5 to 6 months after surgery. However, this does not mean that for 5–6 months a person will feel unwell and will not be able to live and work normally. Full rehabilitation means not only physical and mental recovery from stress and trauma, but also the accumulation of reserves, with which a person will be able to successfully withstand new challenges and stressful situations without harm to yourself and without developing any diseases.
Rehabilitation after laparoscopy of the gallbladder usually proceeds quite quickly and without complications. Complete rehabilitation, including both physical and mental aspects, occurs 5 to 6 months after surgery. However, this does not mean that for 5–6 months a person will feel unwell and will not be able to live and work normally. Full rehabilitation means not only physical and mental recovery from stress and trauma, but also the accumulation of reserves, with which a person will be able to successfully withstand new challenges and stressful situations without harm to yourself and without developing any diseases.
And normal well-being and the ability to perform usual work, if it is not associated with physical activity, appears within 10 - 15 days after the operation. Starting from this period, for the best rehabilitation, the following rules should be strictly adhered to:
- Sexual rest should be observed for one month or at least 2 weeks after surgery;
- Eat right, avoiding constipation;
- Start any sports training no earlier than a month after surgery, starting with minimal load;
- For a month after surgery, do not engage in heavy physical labor;
- During the first 3 months after surgery, do not lift more than 3 kg, and from 3 to 6 months - more than 5 kg;
- For 3–4 months after surgery, follow diet No. 5.
Otherwise, rehabilitation after gallstone laparoscopy does not require any special measures. To speed up wound healing and tissue restoration, a month after surgery, it is recommended to undergo a course of physical therapy, which is recommended by the doctor. Immediately after the operation, you can take vitamin preparations, such as Vitrum, Centrum, Supradin, Multi-Tabs, etc.
Pain after laparoscopy of the gallbladder
After laparoscopy, pain is usually moderate or mild, so it can be easily relieved with non-narcotic analgesics, such as Ketonal, Ketorol, Ketanov, etc. Painkillers are used for 1 to 2 days after surgery, after which there is usually no need for their use , since the pain syndrome decreases and disappears within a week. If the pain does not decrease but intensifies every day after surgery, you should consult a doctor, as this may indicate the development of complications.
After removing the sutures on days 7–10 after surgery, the pain no longer bothers you, but may occur during any active actions, or high voltage anterior abdominal wall (straining when trying to defecate, lifting weights, etc.). Such moments should be avoided. IN long term after the operation (a month or more) there is no pain, and if any appears, this indicates the development of some other disease.
Diet after laparoscopic gallbladder removal (diet after laparoscopy of the gallbladder)
 The diet that should be followed after removal of the gallbladder is aimed at ensuring normal liver function. Normally, the liver produces 600–800 ml of bile per day, which immediately enters the duodenum, and does not accumulate in the gallbladder, being released only as needed (after a bolus of food enters the duodenum). This entry of bile into the intestine, regardless of meals, creates certain difficulties, so it is necessary to follow a diet that minimizes the consequences of the absence of one of the important organs.
The diet that should be followed after removal of the gallbladder is aimed at ensuring normal liver function. Normally, the liver produces 600–800 ml of bile per day, which immediately enters the duodenum, and does not accumulate in the gallbladder, being released only as needed (after a bolus of food enters the duodenum). This entry of bile into the intestine, regardless of meals, creates certain difficulties, so it is necessary to follow a diet that minimizes the consequences of the absence of one of the important organs.
On days 3–4 after surgery, a person can eat pureed vegetables, low-fat cottage cheese, as well as boiled meat and low-fat fish. This diet should be maintained for 3 – 4 days, after which you switch to diet No. 5.
So, diet No. 5 involves frequent and fractional meals (small portions 5–6 times a day). All dishes should be chopped and warm, not hot or cold, and food should be prepared by boiling, stewing or baking. Frying is not allowed. The following dishes and products should be excluded from the diet:
- Fatty foods (fatty fish and meats, lard, high-fat dairy products, etc.);
- Roast;
- Canned meat, fish, vegetables;
- Smoked meats;
- Marinades and pickles;
- Spicy seasonings (mustard, horseradish, chili ketchup, garlic, ginger, etc.);
- Any offal (liver, kidneys, brain, stomachs, etc.);
- Mushrooms in any form;
- Raw vegetables;
- Raw green peas;
- Rye bread;
- Fresh white bread;
- Butter pastries and confectionery (pies, pancakes, pies, pastries, etc.);
- Chocolate;
- Alcohol;
- Cocoa and black coffee.
The following foods and dishes should be included in the diet after laparoscopic gallbladder removal:
- Low-fat varieties of meat (turkey, rabbit, chicken, veal, etc.) and fish (pike perch, perch, pike, etc.) boiled, steamed or baked;
- Semi-liquid porridges from any cereals;
- Soups with water or weak broth, seasoned with vegetables, cereals or pasta;
- Steamed or stewed vegetables;
- Low-fat or skim dairy products (kefir, milk, curdled milk, cheese, etc.);
- Non-acidic berries and fruits, fresh or in compotes, mousses and jellies;
- Yesterday's white bread;
- Jam or jam.
From these products, a diet is compiled and prepared. various dishes, to which you can add 45–50 g of butter or 60–70 g of vegetable oil per day before meals. General daily norm bread consumption is 200 g, and sugar - no more than 25 g. It is very useful to drink a glass of low-fat kefir before bed.
You can drink weak tea, non-acidic juices diluted with water in half, coffee with milk, compote, rosehip infusion. The drinking regime (the amount of water consumed per day) can be different; it should be set individually, focusing on your own well-being. So, if bile is often secreted into the intestines, then you can reduce the amount of water you drink and vice versa.
3 – 4 months after strict adherence to diet No. 5, raw vegetables and unchopped meat and fish are included in the diet. In this form, the diet should be followed for about 2 years, after which moderate amount you can eat everything.
Consequences of gallbladder laparoscopy
 The main unpleasant and causing severe discomfort consequence of laparoscopic removal of the gallbladder is periodic releases of bile directly into the duodenum, which are called postcholecystectomy syndrome. The manifestations of this syndrome are the following symptoms:
The main unpleasant and causing severe discomfort consequence of laparoscopic removal of the gallbladder is periodic releases of bile directly into the duodenum, which are called postcholecystectomy syndrome. The manifestations of this syndrome are the following symptoms:
- Stomach ache;
- Nausea;
- Vomit;
- Rumbling in the stomach;
- Flatulence;
- Diarrhea;
- Heartburn;
- Belching bitter;
- Jaundice and fever (rare).
Unfortunately, the manifestations of this syndrome can bother a person periodically and it is impossible to get rid of them completely for life. If signs of postcholecystectomy syndrome appear, you should switch to strict adherence to diet No. 5, and severe pain should be relieved by taking antispasmodics, for example, No-Shpa, Duspatalin, etc. Nausea and vomiting can be easily relieved with a few sips of alkaline mineral water, for example, Borjomi.
Complications of gallbladder laparoscopy
Directly during the operation The following complications of gallbladder laparoscopy may develop:
- Damage to the blood vessels of the abdominal wall;
- Perforation (hole) of the stomach, duodenum, colon or gallbladder;
- Damage to surrounding organs;
- Bleeding from the cystic artery or from the liver bed.
These complications arise during the operation and require conversion of laparoscopy to laparotomy, which is performed by the surgeon.
Some time after laparoscopy gallbladder, the following complications may occur due to tissue damage and removal of the organ:
- Bile leakage into the abdominal cavity from a poorly sutured stump of the cystic duct, liver bed or common bile duct;
- Peritonitis;
- Inflammation of the tissue around the navel (omphalitis).
Hernia after laparoscopy of the gallbladder
A hernia after laparoscopy of the gallbladder occurs extremely rarely - no more than 5 - 7% of cases. Moreover, as a rule, a hernia occurs in obese people. Also, the risk of hernia formation during laparoscopy of the gallbladder is slightly higher in those people for whom the operation was performed urgently, and not as planned. In general, this complication is rare after laparoscopy.
More about hernias
Laparoscopy of the gallbladder - reviews
 Almost all reviews about laparoscopy of the gallbladder are positive, since people who have undergone this operation consider it to be quite quick, less traumatic and not leading to the need for a long hospital stay. In the reviews, people note that the operation is not scary, it goes quickly and is discharged on the 4th day.
Almost all reviews about laparoscopy of the gallbladder are positive, since people who have undergone this operation consider it to be quite quick, less traumatic and not leading to the need for a long hospital stay. In the reviews, people note that the operation is not scary, it goes quickly and is discharged on the 4th day.
It is worth mentioning separately what unpleasant moments people pay attention to: firstly, it is pain in the abdomen after surgery, secondly, it is difficult to breathe due to compression of the lungs by a gas bubble, which resolves within 2 - 4 days, and finally thirdly, the need to fast for a total of 1.5 - 2 days. However, these unpleasant sensations pass rather quickly, and people believe that they can be endured in order to benefit from the operation.
Cost of laparoscopy of the gallbladder (removal of the gallbladder or removal of stones)
Currently, the cost of laparoscopic removal of the gallbladder or stones from it ranges from 9,000 to 90,000 rubles, depending on the clinic and region of Russia. The most expensive operations are performed in highly specialized medical institutions, such as research institutes. However, city doctors and district hospitals often have no worse experience in carrying out such operations, and their cost is significantly lower.
www.tiensmed.ru
Why is gallbladder removal done?
When contractility the gallbladder decreases or disturbances occur in metabolic processes, bile stagnates. Its components crystallize and precipitate. At first the particles are small (microlites), but gradually they increase in size and turn into stones. Calculous cholecystitis, or cholelithiasis, develops.
The disease has two course options:
- There are stones in the gall bladder, they move, but do not interfere with the flow of bile and do not lead to inflammation.
- Stones disrupt the flow of bile, sometimes move into the bile ducts, block them, cause inflammation and the development of infection.
In what cases is the gallbladder removed? In case of a chronic course, it is not necessary to perform an operation; it is enough to observe changes in the organ and adhere to a certain lifestyle, including nutrition. The risk of complications in this case is low. But this form of the disease can be accompanied by a sluggish inflammatory process, which gradually spreads to other organs. Then the patient, together with the doctor, decides on the operation.
If the outflow of bile is disrupted, inflammation develops, and then infection, then it is almost impossible to eliminate the problem without surgical intervention. The operation to remove the gallbladder is carried out in order to prevent attacks of cholecystitis - colic, accompanied by acute pain, nausea, and vomiting.
In addition, the acute course of the disease leads to complications. There is a risk of spread of inflammatory and infectious processes to the liver, pancreas, and abdominal cavity. The patient may develop reactive hepatitis, cholangitis, pancreatitis, peritonitis, and intestinal obstruction. Pus accumulates in the gallbladder, inflammation intensifies, an abscess covers nearby tissues, and sometimes gangrene or perforation develops in the walls of the organ.
Stages and process of procedure behavior
The gallbladder can be removed during open cholecystectomy or laparoscopy. The first option has more wide list indications, but it is more traumatic. The second one does not require a cavity tissue incision, but in some cases it cannot be used (for example, in case of acute inflammation or adhesions). The choice of method is made by the doctor based on the characteristics of the disease and its complications.
Many patients are concerned about how long the surgery to remove the gallbladder lasts. In both cases, the procedure takes from 30 to 90 minutes. Most often, its duration is 1 hour.
Open cholecystectomy is performed under general anesthesia.

During the operation, the doctor performs the following steps step by step:
- An incision (15-30 cm) is made in the area of the right hypochondrium or midline of the abdomen from the sternum to the navel.
- Ligs the gallbladder using surgical thread.
- It compresses vessels and ducts with special clips.
- The gallbladder is cut off with a scalpel and removed.
- Checks for the presence of stones in the bile ducts.
- Sews up the incision, bringing the catheter out (to remove exudate).
Laparoscopic surgery is also performed under general anesthesia.
The doctor performs the following manipulations:
- A special instrument (trocar) makes 3-4 punctures in the navel area and slightly higher, to the right.
- A probe with a camera is inserted into one of the trocars, the image is displayed on the monitor, and the doctor is able to monitor his actions.
- He inserts clamps through the trocars and places them on the vessels and bile duct.
- Cuts off the gallbladder.
- If the size of the bladder does not allow it to be removed through the hole, then the doctor first removes and removes the stones, and then the organ itself.
- Ultrasound, laser or coagulation stops bleeding.
- He sews up large holes and wounds, seals small ones with adhesive tape.
The surgeon works in a team; some actions can be performed by assistants. The progress of the operation is saved in video format.
Sometimes gallbladder removal is performed on a paid basis; the price of the operation depends on the level of the clinic, region, and the qualifications of the surgeon. On average, it ranges from 20 to 35 thousand rubles, but in some cases it can be much higher.
Postoperative period
When the gallbladder is removed, the patient has many questions about the recovery period, for example, what medications to take, how long to stay in the hospital, and when it will be possible to return to their normal lifestyle.
After open cholecystectomy, the sutures are removed after 6-8 days, and discharge from the hospital occurs on days 10-14, depending on the patient’s condition. You will be able to return to your normal work schedule after 1-2 months.
After laparoscopy, there is no need to remove sutures; you are discharged from the hospital after 2-4 days. After 2-3 weeks you can return to your previous activity.
The recovery period after any type of surgery includes following a diet, a comfortable activity regimen, and massage courses. As for medications, it is sometimes necessary to take mild choleretic drugs.
Complications after surgery
Surgery always carries a risk of complications. Any operation is traumatic, after which problems may arise such as slow healing of wounds, their suppuration, peritonitis, bleeding, internal abscess. Fortunately, the percentage of development of such complications is small.
What else are the risks of removing the gallbladder? Among the most common complaints of patients are pain in the right side, in the liver and stomach, and stool disorders.

Liver pain
For the most part the liver is located with right side: from the diaphragm (nipple level) to the lower edge of the ribs. For one and a half months after the gallbladder is removed, the liver may hurt. If the sensations are tolerable and are not accompanied by other symptoms, then this is normal. In this way, the body adapts to the changes that have occurred. If nausea, vomiting, fever, or digestion problems occur, you should consult a doctor.
After surgery, the liver still produces bile. Most often, it goes directly into the intestines, but in some cases, when the gallbladder is removed, the bile ducts can become clogged with secretions, causing symptoms of cholestasis to develop: Blunt pain in the right hypochondrium, jaundice skin and sclera, nausea, bitterness in the mouth, lethargy, drowsiness.
If the gallbladder is removed and the liver hurts, stagnation of bile is confirmed by the results of a biochemical blood test and treatment is prescribed: taking drugs with hepatoprotective and choleretic effects (Essentiale, Ursosan, Liv 52, etc.). Gradually, the body adapts to the changes, and the intrahepatic ducts partially replace the gallbladder without pain.
Pain in right side
After the gallbladder is removed, patients often experience pain on the right side.
This symptom can be caused by several reasons:
- Damage to soft tissue during surgery and subsequent inflammation. Even with laparoscopy, wounds cannot be avoided; until they are completely healed, pain may be felt in the right side.
- Adaptation of the digestive system to changed conditions. The pain is mild, does not require treatment, and disappears after 1-1.5 months.
- Development of new and exacerbation of chronic diseases of the gastrointestinal tract: pancreatitis, hepatitis, duodenitis, gastric and duodenal ulcers, spasm of the bile ducts, biliary dyskinesia, etc.
- Dietary disorder. Digesting spicy, fatty, too sour or salty foods requires a lot of bile. Since the gallbladder is no longer there, the body cannot provide it in sufficient quantities. Digestive disorders manifest themselves as pain.
- Residual stone– the cause of biliary colic when the gallbladder is removed. During the operation, a small stone in the duct may go unnoticed. Subsequently, its displacement causes pain.
In order to determine what exactly caused the pain in the right side, you need to consult a doctor. He will conduct an examination and, if necessary, prescribe treatment.
Stomach ache
When the gallbladder is removed, patients often complain of stomach pain. This unpleasant symptom is associated with changes occurring in the digestive system. After the operation, bile does not accumulate, and therefore its consistency and composition change: it becomes liquid, less active in relation to pathogenic microflora, but aggressively affects the mucous membrane of the duodenum.
As a result, the motility of this section is disrupted, and food masses are thrown back into the stomach cavity and into the esophagus. Pain appears, gastritis, colitis, and enteritis develop. This condition requires consultation with a gastroenterologist.

Stool disorder
When the gallbladder is removed, digestive disorders may appear, which are often manifested by loose stools, less often by constipation. Diarrhea develops due to the rapid passage of bile acids through the duodenum and stimulation of production digestive juice ahead of time.
Another reason loose stool is a violation of the intestinal microflora. As noted earlier, bile becomes less concentrated and has a worse effect on pathogenic microflora. The situation is aggravated by a decrease in the body’s immune forces due to the operation. Bacterial overgrowth syndrome develops, accompanied by periodic diarrhea, bloating and flatulence.
Due to exposure bile acids irritation of the duodenum appears on the mucous membrane. The absorption of vitamins, minerals and nutrients is impaired. The stool may become watery, foul-smelling, or “greasy” or oily (if fat absorption is impaired).
The cause of constipation after gallbladder removal is most often a decrease in the amount of food consumed and the lack of fiber products in it. Therefore, it is important to follow the recommended diet and water regime.
Nutrition after surgery
After removal of the gallbladder, the functioning of the gastrointestinal tract changes. If previously the release of bile occurred after food intake, now it flows constantly in small portions. This leads to irritation of the mucous membrane, inflammation, and impaired motility of the duodenum. Changes in the composition of bile also negatively affect the process of digestion of food.
Correcting your diet helps you avoid many digestive problems and diseases of the gastrointestinal tract.
General rules are:
- During the day you need to drink about 2 liters of water, including 1 glass before each meal.
- All food and drinks should be taken warm, the optimal temperature is about 35-40° C. Hot and cold are prohibited.
- To ensure that bile is removed from the body and does not irritate the intestinal mucosa, you need to eat as often as possible, 5-7 times a day. Portions may be small.
- Cooking and stewing are permitted methods of cooking. When frying, compounds are formed in the dish that provoke intense secretion of gastric juice, which leads to irritation of the mucous membrane and disruption of its functioning.
After removal of the gallbladder, you will have to give up strong coffee and tea, soda and alcohol, most sweets, legumes, mushrooms, sausages, canned food and smoked meats. All foods high in animal fat are prohibited: some types of fish, poultry, meat, lard. When preparing dishes, you should not add spices (especially hot ones), onions and garlic. Use salt to a minimum; it is best to add it to already prepared food.
Allowed recipes for gallbladder removal:
- soups based on vegetable, fish or low-fat meat broth;
- fish, poultry, beef or veal, steamed, boiled or stewed;
- Buckwheat and oatmeal are the most preferred side dishes; semolina should be avoided;
- for dessert you can prepare baked or stewed fruits;
- stewed, steamed or boiled vegetables;
- cottage cheese 9% fat, kefir, yogurt, fermented baked milk, bifidok - always fresh.

This diet is called “Table No. 5”. It is designed specifically for patients with liver and gallbladder diseases. 2 months after the operation, fats can be introduced into the diet: vegetable oils, small amounts of butter and sour cream. If you want something sweet, you are allowed to eat a little honey, marshmallows, marmalade, and dry cookies, but all this should be without cocoa, chocolate, nuts or seeds.
The gallbladder is not a vital organ. With the spread of inflammatory and infectious processes not only its work is disrupted, but there is also a danger of developing complications - diseases of organs located nearby. Indications for removal of the gallbladder are the presence of stones in it, a violation of the outflow of bile, the development of inflammation and infection.
Medicines are not effective enough because they are unable to eliminate stones. Surgery to remove the gallbladder can be performed traditionally (open cholecystectomy) or laparoscopically. The second option is less traumatic, but in some cases cannot be used.
When a person has his gallbladder removed, he has a question: how to live after the operation? Activity restrictions will need to be observed for 1.5-2 months. A diet that helps the digestive organs adapt to changes - about a year. Otherwise, you don’t have to change your lifestyle.
moizhivot.ru
Preparation for laparoscopy of the gallbladder
Actions necessary in preparation for laparoscopy:
- mandatory shown ultrasonography abdominal cavity;
- blood analysis;
- chest x-ray;
- medical examination;
- making a surgical verdict for the operation;
- cleansing the large and small intestines;
- before the operation, you cannot drink or eat from 12 o’clock at night (except for necessary medications);
- a few days before surgery, stop taking anti-inflammatory drugs, vitamin E, aspirin, and anticoagulants.
Gallbladder surgery (laparoscopy)
Laparoscopy of the gallbladder is performed under general anesthesia (anesthesia) in a special hospital, and lasts approximately one hour.
After preparing the surgical field, the surgeon makes four punctures in the abdominal wall, into which trocars (metal conductors in the form of hollow tubes) are inserted.
Sterile carbon dioxide is pumped into the abdominal cavity from cylinders, creating a working space for the surgeon to operate. Through one trocar (puncture), a laparoscope with a video camera and a light source is inserted. Color image from the video camera goes to the monitor.

The surgeon’s endoscopic special instruments are inserted into other trocars:
- grips;
- forceps;
- coagulators;
- scissors;
- clamps.
After laparoscopy of the gallbladder, staples are applied to the blood vessels and bile ducts.
Bile is then sucked out of the gallbladder through a puncture. The bubble decreases in size, deflates, and is now easy to remove through the conductor.
The punctures in the abdominal wall are sutured, and the patient is sent for further observation and rehabilitation to the hospital for several days (3-5). The patient is then assigned a restriction physical activity and a special diet.
Nutrition after laparoscopy of the gallbladder should contain restrictions on the following products:
- alcohol;
- flour products;
- fried and fatty foods.
Indications for laparoscopy of the gallbladder
The main indication for cholecystectomy is calculous cholecystitis (inflammation of the gallbladder).
Typically, the inflammatory process in the gallbladder occurs in the presence of stones (calculi), consisting of dense crystalline formations of cholesterol.
Contraindications to laparoscopy of the gallbladder
Some clinical cases require a transition to classical open surgery when performing endoscopic intervention:
- the presence of scars and adhesions on the walls of the abdominal cavity after previous surgical operations;
- high degree of obesity;
- high blood loss during laparoscopy;
- large and numerous stones in the gall bladder;
- abscess in the gallbladder area;
- poor visibility of anatomical structures in the laparoscopy area;
- cardiovascular diseases;
- diseases of the respiratory system at the stage of decompensation;
- last trimester of pregnancy.
Benefits of gallbladder laparoscopy
The main advantages include:
- four small punctures on the abdomen, instead of a 15-centimeter incision;
- minimal pain after surgery;
- faster recovery of the body after laparoscopy;
- faster return to normal physical activity.
The temperature after laparoscopy of the gallbladder usually stays around 37-39 degrees for about seven days. About a week after the operation, the patient is fully recovered and recovering.
Complications after laparoscopy of the gallbladder
Most severe consequences after the operation:
- bile leakage;
- intra-abdominal bleeding;
- subphrenic abscesses;
- subhepatic abscesses;
- inflammatory process in the wound of the abdominal wall.
The gallbladder is an important organ that plays an important role in the digestive process.
Liver cells - hepatocytes - secrete a special substance called bile. The gallbladder is a kind of reservoir for storing this substance.
When food arrives, the organ releases bile through the ducts into the intestines for the further digestion process.
Removal of the gallbladder is a common operation that is performed when pathological problems with this organ.
Reasons for the formation of pathologies
The main problem for which surgery to remove the gallbladder is stone formation. There are many factors.
It should be noted that if previously such a problem occurred in older age, now stones can appear even in children.
Often this is due to poor nutrition. Nowadays there is a large assortment on store shelves and they are not always of high quality and healthy foods. Parents eat themselves and feed it to their children, and as a result, various problems occur.
Stone formation occurs when cholesterol levels rise in the body. Products with a high content of it: butter, fatty meat, eggs, kidneys, etc.
Also, problems are provoked when people do not have a specific routine. Or, if long fasting gives way to overeating. In this case, a person tries to saturate his body with fried, fatty or sweet foods.
As a result, as a result, a person who abuses junk food becomes obese. It is very bad when fatty liver degeneration develops.
In addition to poor diet, there are other reasons for the formation of gallstones.
This could be taking medications. Especially if the dosage is exaggerated or the course is not followed. This also applies to hormonal contraceptives.
The appearance of the disease is also influenced by other pathological changes in the organ. Various kinks, folds and other anatomical changes can provoke the development of stone formation.
Sometimes, complete removal of the gallbladder is the only correct solution. It is important that the operation is performed by a qualified specialist in order to prevent the possibility of various complications.
Indications for surgery
There are several ways to remove an organ. Depending on the course of the disease and the type of pathology, one or another method is used.
Indications for surgery are:
- Gallstone disease. It is with this disease that cholecystectomy is most often required. Most often it is characterized by frequent attacks of biliary colic. This greatly complicates the lives of patients, and they already agree to anything just to end their torment. In addition, the development and growth of stones in the gallbladder and its ducts leads to various complications. If treatment is not started in time, a person may develop peritonitis or rupture of the gallbladder. And this is fraught fatal. In humans, the disease may be accompanied by: severe symptoms, or their complete absence. In any case, the purpose of the operation is to prevent complications.
- Polyposis. Periodic examination is necessary if polyps are detected in the organ. Indications for removal are: rapid growth (if the size exceeds 10 mm and the polyp stalk is thin), combination with cholelithiasis.
- Cholesterosis with poor flow of bile. Its accompanying stone formation in the gallbladder is considered dangerous. Also, the operation must be carried out without fail if calcium salts are deposited on the walls of the organ. It may be accompanied by symptoms or occur in a quiet form, without showing any signs.
- Acute and chronic inflammation of the gallbladder. For example, this is cholecystitis. The disease is characterized severe inflammation walls of the gallbladder. It is especially dangerous when cholecystitis is accompanied by the presence of stones. In this case, the operation should be carried out as soon as possible.
- Other functional disorders of the organ, when conservative treatment is impossible and there is a risk of complications.
Contraindications
If there are contraindications, the specialist chooses what poses the greatest risk to human health.
Therefore, only some caution is observed on the part of the doctor. All contraindications can be divided into local and general.
General contraindications:
- Exchange disorders.
- Terminal states.
- Severe decompensated pathology of internal organs.
Laparoscopy is not advisable if:
- Late pregnancy.
- Pathological problems of internal organs at the stage of decompensation.
- Pathology of hemostasis.
- Peritonitis.
Local contraindications for laparoscopy:
- Adhesive disease.
- Acute cholecystitis.
- Pregnancy 1st and 3rd trimester.
- Formation of calcium salts on the walls of the gallbladder.
- Large hernias.
In this case, the doctor and patient must consider all the risks and make an important decision. If laparoscopy is not possible, then abdominal surgery is performed.
What awaits the patient after surgery?
Any intervention causes various changes. Surgery to remove the gallbladder is no exception.
The patient can live a completely normal life without the presence of this organ. But at the same time, you will need to follow all the specialist’s recommendations, and also be sure to monitor your diet and give up bad habits.
Only in this case can a person count on a full and high-quality life.
But even with the most positive course of the postoperative period, transformation occurs inside the body.
Changes in the body after removal:
- Bile was involved in digestion and helped fight accidentally ingested bacteria and harmful components. After removal of the organ, the intestinal microflora will change and the bacterial population will increase.
- Now there is no place to store bile, which means it will go straight from the liver straight to the intestines.
- The intracavitary pressure on the hepatic ducts will increase.
Provided that the person does not follow a diet and consume fatty foods, there is a lack of bile for digestion.
As a result, various disorders are observed in the intestines, food absorption slows down and worsens.
The patient begins to experience the following symptoms:
- Nausea. In some cases, the body may even begin to reject food, which will manifest itself in the form of vomiting. Bile is present in the vomit.
- Increased gas formation.
- Signs of indigestion.
- Heartburn.
In this situation, the patient experiences a lack of certain substances in the body:
- Antioxidants.
- Fatty acid.
- Vitamins A, E, D, K.
The composition of bile also plays an important role. During the rehabilitation period, the patient is prescribed special treatment, which normalizes the state of bile juice.
If its effect is too caustic, serious damage to the intestinal mucosa is possible. As a result, there is a risk of cancer formation.
Feelings in the first days after cholecystectomy
Much will depend on the patient’s body and on the methods of performing the operation. With laparoscopy, a person recovers within 2 weeks.
When surgery was performed using the usual abdominal method, rehabilitation time is about 8 weeks.
In the first days after surgery, the patient may have the following symptoms:
- Nausea. Its appearance is most often influenced by the effects of anesthesia.
- Pain at the site of the incision or puncture. This is a natural manifestation, because a person has just lost a very important organ. Doctors prescribe various painkillers for pain.
- After laparoscopy, there may be pain in the abdominal area, radiating to the shoulders. They should disappear in a few days.
- General malaise.
- Gas formation.
- Diarrhea.
This is a natural process of adaptation. For some, the symptoms may expand, while for others it will be limited to a couple of signs.
The main thing is that the person does not panic and follows all the doctor’s recommendations without exception.
Standard abdominal surgery
This surgical intervention involves a midline laparotomy or oblique incisions under the costal arch.
This allows the specialist to gain good access to the organ and its ducts.
Open surgery has a number of disadvantages:
- Large seam, which does not look the best.
- Major surgical trauma.
- There is a high probability of complications. Most often these are functional failures in the intestines and other internal organs.
The main indications for abdominal surgery serve:
- Acute inflammatory process with peritonitis.
- Complex lesions of the bile ducts.
Operational stages:
- An incision into the anterior wall of the peritoneum and a full examination of the work to be done.
- Isolation and ligation of all ducts and arteries leading to the organ to prevent bleeding.
- Removing the gallbladder.
- Processing the location of the organ.
- Applying drainage and suture to the incision site.
Laparoscopy
The most adequate treatment for many problems in the gallbladder. This method has many advantages compared to the cavity method.
Firstly, laparoscopy causes minor surgical trauma. Secondly, it causes minor pain syndrome in patients during the rehabilitation period. Thirdly, laparoscopy has a short recovery period.
After such treatment, the doctor can discharge the patient from the hospital on day 3, provided there are no complications.
Indications for use:
- Chronic form of cholecystitis.
- Cholelithiasis.
- Acute inflammatory processes in the gallbladder.
Operational stages:
- Laparoscopy involves inserting a series of instruments directly into the gallbladder. The entire procedure is performed using a computer monitor. The operation must be performed by a qualified specialist. At the first stage, punctures of the abdominal wall and insertion of instruments are performed.
- To ensure a better overview, carbon dioxide is pumped into the abdomen.
- Next comes clipping, cutting off ducts and arteries.
- The removal of the organ itself.
- Removal of instruments and suturing.
The speed of the operation is noted. Very often, laparoscopy takes no more than 1 hour, and only in some cases, if complications arise, it lasts up to 2 hours.
It should be noted that it is impossible to remove large stones through punctures. To do this, they are first crushed and only then removed from the gallbladder in small parts.
Sometimes it is necessary to install drainage under the liver. This is done to ensure the outflow of bile that has formed due to surgical trauma.
Mini access
Another way to remove the gallbladder. If laparoscopy is not possible due to some contraindications, the doctor decides to change the method of surgical intervention. One of these is the minimally invasive method.
Mini access is something between a conventional operation and laparoscopy. Operational stages include:
- Providing access.
- Ligation and cutting of arteries and ducts.
- Removal of the gallbladder.
Unlike simple abdominal surgery, mini-access is characterized by a small incision area. The incision is made no more than 7 cm under the ribs on the right side.
This method of operation allows the surgeon to inspect the insides and extract the gallbladder as efficiently as possible.
Indications for minimally invasive surgery:
- The presence of a large number of adhesions.
- Inflammatory tissue infiltration.
The patient is discharged from the hospital on the 5th day after surgery. Compared with abdominal surgery, the postoperative period is much easier and faster.
Preparing for surgery
How the removal itself and the rehabilitation period will go will depend on how the patient prepares for the operation.
Before the operation, diagnostic measures must be prescribed:
- Coagulogram.
- Blood analysis. They do both general and biochemical. It is also important to identify the presence of syphilis and hepatitis.
- Analysis of urine.
- Fluorography of the lungs.
- Ultrasound diagnostics of abdominal organs.
- It is important to find out your blood type and Rh factor before surgery.
- Fibrogastroscopy.
- Colonoscopy.
It is also necessary to undergo examination and obtain advice from various specialists. Everyone should consult a physician. Some need to visit a gastroenterologist, endocrinologist, or cardiologist.
Before proceeding with the operation, specialists must identify all contraindications and clarify various important points.
You also need to bring your blood pressure back to normal and monitor your sugar levels if the patient is diabetic. Severe pathologies of internal organs should be compensated as much as possible.
You need to adapt to a special diet in advance. On the eve of the operation, food should be as light as possible.
Already in the evening before the operation, the patient is deprived of any food and water. Also in the evening and in the morning, a person is given a cleansing enema to eliminate any contents inside the intestines.
In case of an acute course and sudden hospitalization, the procedures are carried out very quickly. All procedures take no more than 2 hours.
Postoperative period
How long a person will be in the hospital depends in most cases on the type of surgery. How the body will recover is directly related to compliance with the recommendations and the condition of the body itself.
During abdominal surgery, the sutures are removed no earlier than 7 days, and the patient is kept under control for about 2 weeks. With a good course and restoration of the body, the ability to work occurs within 1-2 months.
Laparoscopy is less traumatic and a person is discharged within 2-4 days. A person also recovers much faster. Full working capacity occurs after 20 days.
For the first 6 hours you should not consume food or water. It is also worth observing bed rest. On the first day, a person may experience nausea and dizziness.
This is a natural state, because the patient is recovering from anesthesia. Therefore, the first attempts to get out of bed should be careful.
Only after a day, the patient is allowed to walk around the room a little, drink and eat. The diet includes: bananas, cereals, vegetable purees, light soups, boiled lean meats, dairy products.
The following are prohibited: various sweets and pastries, strong tea, coffee, fried and spicy foods, alcohol.
Diet is now important companion person after cholecystectomy. Now the body is losing an important organ, and the load increases noticeably. To reduce the impact of negative factors, experts advise following diet No. 5.
Your doctor may also prescribe medications containing enzymes that improve digestion. These are Pancreatin, Mezim, Festal. The use of choleretic herbs will also be useful.
Useful video

















 Stages of laparoscopic surgery include:
Stages of laparoscopic surgery include:

 A day after the operation, you are allowed to stand up, walk around the room, and take food and water. The diet after removal of the gallbladder is of particular importance. In the first few days you can eat porridge, light soups, fermented milk products, bananas, vegetable purees, and lean boiled meat. Coffee, strong tea, alcohol, confectionery, fried and spicy foods are strictly prohibited.
A day after the operation, you are allowed to stand up, walk around the room, and take food and water. The diet after removal of the gallbladder is of particular importance. In the first few days you can eat porridge, light soups, fermented milk products, bananas, vegetable purees, and lean boiled meat. Coffee, strong tea, alcohol, confectionery, fried and spicy foods are strictly prohibited. The term “gallbladder laparoscopy” in everyday speech usually means an operation to remove the gallbladder, performed using a laparoscopic approach. In more rare cases, this term may mean that people are removing stones from the gallbladder using laparoscopic surgery.
The term “gallbladder laparoscopy” in everyday speech usually means an operation to remove the gallbladder, performed using a laparoscopic approach. In more rare cases, this term may mean that people are removing stones from the gallbladder using laparoscopic surgery. Currently surgery to remove gallstones is almost never performed for two main reasons. Firstly, if there are a lot of stones, then the entire organ should be removed, which is already too much pathologically changed and therefore will never function normally. In this case, removing only the stones and leaving the gallbladder is unjustified, since the organ will constantly become inflamed and provoke other diseases.
Currently surgery to remove gallstones is almost never performed for two main reasons. Firstly, if there are a lot of stones, then the entire organ should be removed, which is already too much pathologically changed and therefore will never function normally. In this case, removing only the stones and leaving the gallbladder is unjustified, since the organ will constantly become inflamed and provoke other diseases. Laparoscopy has the following advantages over major abdominal surgery:
Laparoscopy has the following advantages over major abdominal surgery:
 Indication The following diseases require removal of the gallbladder using the laparoscopic method:
Indication The following diseases require removal of the gallbladder using the laparoscopic method: Rehabilitation after laparoscopy of the gallbladder usually proceeds quite quickly and without complications. Complete rehabilitation, including both physical and mental aspects, occurs 5 to 6 months after surgery. However, this does not mean that for 5–6 months a person will feel unwell and will not be able to live and work normally. Full rehabilitation means not only physical and mental recovery from stress and trauma, but also the accumulation of reserves, with which a person will be able to successfully withstand new challenges and
Rehabilitation after laparoscopy of the gallbladder usually proceeds quite quickly and without complications. Complete rehabilitation, including both physical and mental aspects, occurs 5 to 6 months after surgery. However, this does not mean that for 5–6 months a person will feel unwell and will not be able to live and work normally. Full rehabilitation means not only physical and mental recovery from stress and trauma, but also the accumulation of reserves, with which a person will be able to successfully withstand new challenges and  The diet that should be followed after removal of the gallbladder is aimed at ensuring normal liver function. Normally, the liver produces 600–800 ml of bile per day, which immediately enters the duodenum, and does not accumulate in the gallbladder, being released only as needed (after a bolus of food enters the duodenum). This entry of bile into the intestine, regardless of meals, creates certain difficulties, so it is necessary to follow a diet that minimizes the consequences of the absence of one of the important organs.
The diet that should be followed after removal of the gallbladder is aimed at ensuring normal liver function. Normally, the liver produces 600–800 ml of bile per day, which immediately enters the duodenum, and does not accumulate in the gallbladder, being released only as needed (after a bolus of food enters the duodenum). This entry of bile into the intestine, regardless of meals, creates certain difficulties, so it is necessary to follow a diet that minimizes the consequences of the absence of one of the important organs. The main unpleasant and causing severe discomfort consequence of laparoscopic removal of the gallbladder is periodic releases of bile directly into the duodenum, which are called postcholecystectomy syndrome. The manifestations of this syndrome are the following symptoms:
The main unpleasant and causing severe discomfort consequence of laparoscopic removal of the gallbladder is periodic releases of bile directly into the duodenum, which are called postcholecystectomy syndrome. The manifestations of this syndrome are the following symptoms: Almost all reviews about laparoscopy of the gallbladder are positive, since people who have undergone this operation consider it to be quite quick, less traumatic and not leading to the need for a long hospital stay. In the reviews, people note that the operation is not scary, it goes quickly and is discharged on the 4th day.
Almost all reviews about laparoscopy of the gallbladder are positive, since people who have undergone this operation consider it to be quite quick, less traumatic and not leading to the need for a long hospital stay. In the reviews, people note that the operation is not scary, it goes quickly and is discharged on the 4th day.